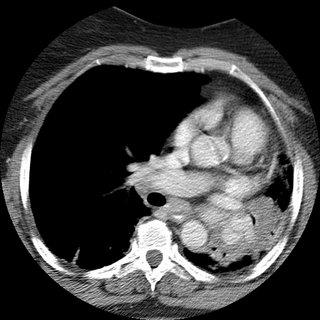
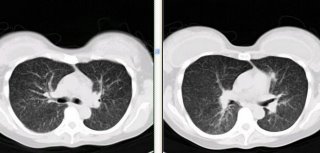
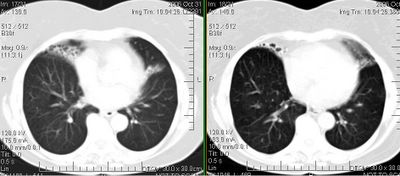
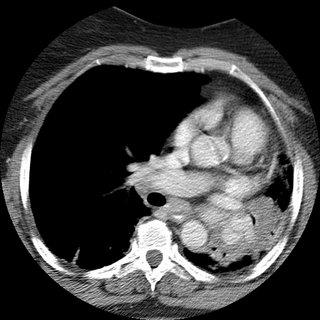
62 woman c/o 2 weeks ago started to have cough with greenish sputum. She presented to the ER where workup included a CT (below).
Pt states that was diagnosed with asthma in 2002; at that time she had a CXR that showed scar tissue in the left upper lobe secondary to a previous pneumonia.
She noticed that over the last year, she has being unable to lay down over her right side because she would feel short of breath, so that she always sleep over her left side. Denies frequent cough, sputum production, hemoptysis, weight loss, loss of appetite, chronic chest pain.
SOCIAL HISTORY:
pt has 40 pack year history of smoking, quit in 1998. She works as hair stylist and is exposed to fumes and chemicals. Denies exposure to TB. No recent travels.
PHYSICAL EXAM:
BP 139/83, HR 86x', RR 16x', O2Sat 93% on RA, W 212 pounds.
Patient is awake, alert, obese, oriented x3, no acute distress.
Neck, no lymphadenomegaly. Chest, no use of accesory muscles, no retractions, flat to percussion on the left, no prolonged expiration, absent breath sounds in the left, no wheezes, no crackles. CV: regular rhythm, no S3 or S4, no murmurs. No rubs.
Spirometry showed severe obstruction.
(quick) DDx and how would you proceed?