77 year old admitted a year ago with pneumonia and referred for lung nodules. He had a PPD placed for unknown reasons in December, (no TB risks/exposures) that is 18 mm induration.
A CT is here: 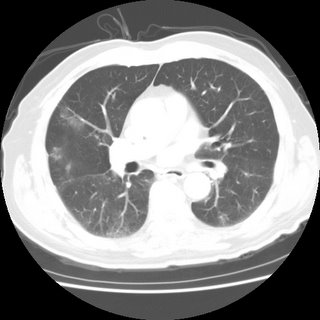 7 mm nodule
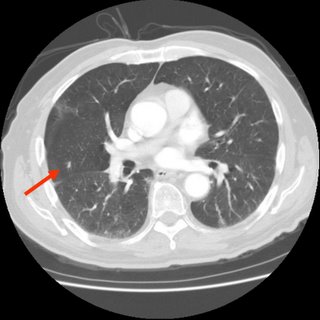
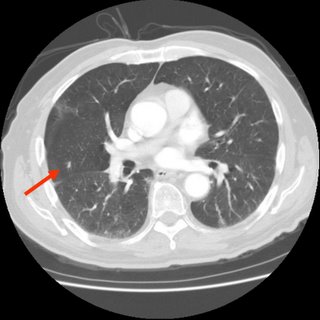
7 mm nodule:
He has no respiratory or constitutional symptoms. Is there anyone that would
not do a BAL to rule out active TB prior to treating for latent?
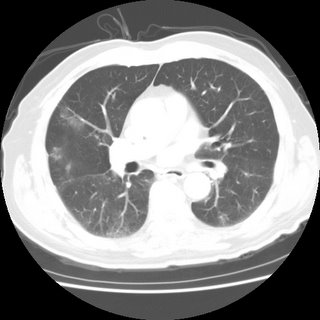
Those are very subtle findings... any mediastinal/hilar adenopathy? Any calcified granulomata? Are those little infiltrates present in other cuts?
ReplyDeleteThere is a 7 mm nodule in upper lobe that is new. There is no adenopathy.
ReplyDeleteI added the nodule slice to the post.
Nothing calcified.
The rest of the CT is pretty unremarkable.
Does he have any old PPDs?
ReplyDeleteI don't think this is active TB. The radiographic changes are very subtle and if he had air-space dz with TB with no old calcified changes (hence, fairly acute disease) I would expect more symptoms. It sounds from your description that he doesn't even have a cough...
Now, having said that I think you are kind of stuck digging a little deeper: if you start INH for LTBI and those changes turn out to be atypical TB he will get a resistant bug. If you start 4 drugs for therapy and he is not coughing, you will not have any cultures and he will be stuck on 4 drugs with side effects for 6 months.
I would consider one of 2 things: a bronch as you suggested or, give him a quick course of "regular" ABTx and repeat a CT in 4 weeks. If it resolves or improves and he does not have symptoms of active TB you would have an alternative explanation and could go ahead with Tx for LTBI.
I like the bronch optin best because you can r/o active TB right away instead of waiting 4 weeks. I agree tht the pre-test prob for active TB is low, but with no known previous PPD (and now 18 mm) and a new 7 mm RUL nodule with some ground lass-ish in the middle, I thought it would be best to do a quick BAL...
ReplyDeleteI think a combination approach is reasonable. Do a bronch to get the samples, and re-image in 6 weeks if the bronch is negative. Then, treat for LTBI and, if the radiographic lesions progress, consider further diagnostic evaluation for non-TB disease.
ReplyDelete