This is a 77 y/o woman with no previous label of chronic lung disease. She had rheumatic fever and hystoplasmosis in the 50's, has mild HTN but is otherwise fairly healthy.
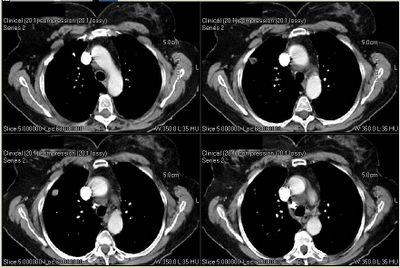
She was sent to me for a pre-op evaluation: prior to total knee replacement she had a CxR that revealed "a lesion". A CT scan was performed and revealed a pulmonary nodule (see below).
She has no cough, no fever/chills/night sweats. Surgery was scheduled for the day after her consult with me.
PMHx: as above. Only meds are anti-HTN.
SHx: She has never smoked. No ETOH, no IVDA. No occupational exposures. Her husband was a heavy smoker and died of lung Ca and COPD.
FHx: No Hx of solid organ tumors.
ROS: non-contributory.
Fairly normal exam, slightly overweight but clear lungs.
Full PFTs were normal (good flow-volume loop).
CT scan showed only the nodule seen below.
She is clearly OK to go through surgery from a respiratory "mechanic" point of view. But what would you do with the nodule? How would you time your work up.
6 comments - CLICK HERE to read & add your own!:
Nice case.
I think I would probably talk to her about the need to go after the nodule before she gets her knee fixed.
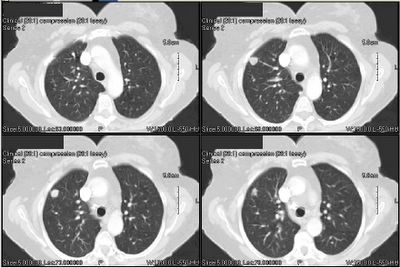
The survival from a stage I (this looks like a T1N0M0, but my views of the CT scan are poor at best) bronchogenic carcinoma is pretty good, but deteriorates rapidly as the stage increases.
Peripheral nodules can be adenoCA, and still scare me. Histoplasmosis can leave nodules, but to me, this is cancer until prove otherwise.
I suppose you could PET the nodule and see if it is hot. The surgeons here like it to see if they need to do mediastinoscopy on the table before the lobectomy.
So, my plan: PET scan, surgery if the nodule is hot. long discussion at thoracic oncology conference if it is not, and delay the knee surgery for the time being.
Well, on the one hand she has good lung function and you have a solitary, non-calcified nodule so resection would be a possibility.
On the other hand the patient is a lifelong nonsmoker, does not have COPD by spiro and has a lesion that is quite peripheral with fairly smooth borders to it.
For this reason, I might obtain a PET. I realize that carcinoid and bronchoalveolar cancers are PET negative (and happen in nonsmokers),
but if positive take it out, if negative repeat in 3 months and take out if growing.
The knee surgery is elective so would hold off on that at least until the pet comes back.
Although, for diagnosis PET scan may be very helpful, I would use it for staging purposes. I believe this lady has enough risk factors for cancer (age, heavy second-hand smoking, lack of calcification and size) and I would not hesitate to perform an excisional biopsy; however, if metastatic disease exists my approach would change.
I'd do a staging PET. If the nodule is hot and the mediastinum is clear, it comes out. If the mediastinum and the nodule are hot, than a bronch with Wang or a mediasteinoscopy are needed. If the the nodule is cold, agree with long discussion as resection or three month follow-up are reasonable depending on the patient's preference.
It is interesting haow we have all thought about using PET as a tie-breaker. It is also interesting that SPN algoriths (such as from http://www.chestx-ray.com/SPN/SPNProb.html) don't have an entry for second-hand smoking. If you enter har data as a non-smoker (SHE has never smoked) the probability of malignacy adds up to 26-27%.
I had a long discussion with the patient and presented the same options you have suggested. She still wanted to have the knee fixed. That was done the very next day. We are getting a PET and shwill then see the surgeons. I will keep you updated as a separate post.
Uh...everything you have all mentioned is expensive, her risk of malignancy is low, she's already had histo (lives in histo belt?) Sorry, but somebady has to state the obvious. Old films, anyone.
Post a Commenttest post a comment