Wednesday, August 31, 2005
Valley Fever
73 yo female with PMH of thoracic aortic aneurysm being followed with serial CT scans. She spends the winter months in Arizona and was admitted to an OSH with dyspnea and respiratory failure. She presented with no records, so I relied on her memory (which was surprisingly good).
Her hospital course was complicated by VDRF requiring about 2 weeks on the vent. A BAL of her LLL was performed and yielded (per her report) "Valley Fever." She was placed on fluconazole (unknown dose). Her chest xray showed lobar pneumonia. PPD negative at OSH; BAL neg for AFB.
She slowly recovered and presented to my office 8 months later with dyspnea, fatigue and chest pain. She was being treated with Fluconazole 100 mg daily and had been on that dose for the last few months.
Her chest pain was typical for cardiac, so I got a functional study of her heart. It was positive. A cath was performed by cardiology and a PTCA/stent was placed in her PDA; her symptoms clearly improved. However, she was not back at her baseline.
PMH: CAD, Thoracic Aortic aneurysm (stable x 4 years), HTN, hyperlipidemia, obesity (182 lbs; 5"3')
SH: no tob, etoh, drugs, travel (other than arizona)
PE: sat 93% on RA; o/w unremarkable
PFT's: FEV1 1.60 (77%)
FVC 2.04 (74%)
FEV1/FVC 79% (105%)
TLC 4.51 (92%
RV 49 (109%)
DLCO 10.28 (45%)
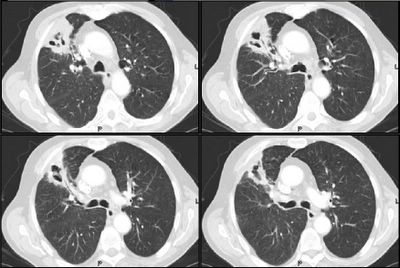
Radiographs:

Chest CT's in the past (i.e. before her trip to Arizona) do not show any pulmonary abnormalities. She has gotten serial Chest CT's to follow her aneurysm.
What would you do next?
Her hospital course was complicated by VDRF requiring about 2 weeks on the vent. A BAL of her LLL was performed and yielded (per her report) "Valley Fever." She was placed on fluconazole (unknown dose). Her chest xray showed lobar pneumonia. PPD negative at OSH; BAL neg for AFB.
She slowly recovered and presented to my office 8 months later with dyspnea, fatigue and chest pain. She was being treated with Fluconazole 100 mg daily and had been on that dose for the last few months.
Her chest pain was typical for cardiac, so I got a functional study of her heart. It was positive. A cath was performed by cardiology and a PTCA/stent was placed in her PDA; her symptoms clearly improved. However, she was not back at her baseline.
PMH: CAD, Thoracic Aortic aneurysm (stable x 4 years), HTN, hyperlipidemia, obesity (182 lbs; 5"3')
SH: no tob, etoh, drugs, travel (other than arizona)
PE: sat 93% on RA; o/w unremarkable
PFT's: FEV1 1.60 (77%)
FVC 2.04 (74%)
FEV1/FVC 79% (105%)
TLC 4.51 (92%
RV 49 (109%)
DLCO 10.28 (45%)
Radiographs:
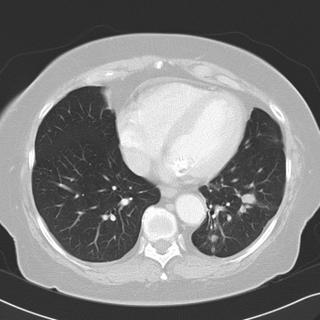

Chest CT's in the past (i.e. before her trip to Arizona) do not show any pulmonary abnormalities. She has gotten serial Chest CT's to follow her aneurysm.
What would you do next?
Tuesday, August 30, 2005
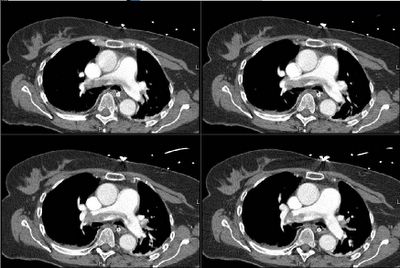
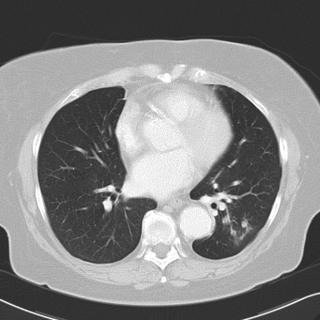
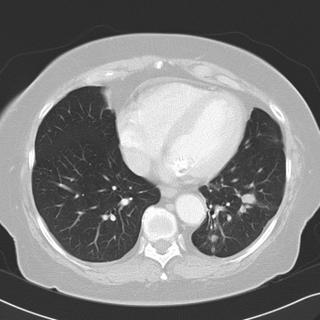
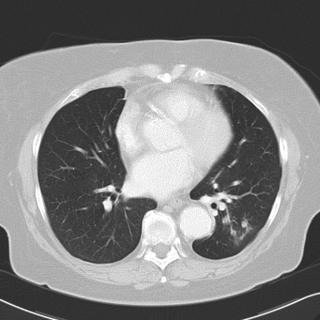
Abnormal CT scan
This is a 68 y/o man with COPD, still smoking with a persistent cough. No hemoptysis, no sputum production. His Cxr at his PCP's was abnormal and he came to us with the following CT scan.
SHx:>50 p/year TOB.
Exam showed only hyperinflation and minimal crackles in the R mid lung field.
FVC is 70% and FEV1 is 54%.
What is your differential and how would you proceed from here?
SHx:>50 p/year TOB.
Exam showed only hyperinflation and minimal crackles in the R mid lung field.
FVC is 70% and FEV1 is 54%.
What is your differential and how would you proceed from here?
Monday, August 29, 2005
Solitary Lesion
Okaaayy...Any hoo, I guess I will post my case (is this on?).
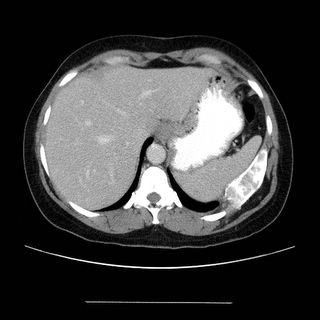
70 year old previous 30+ pack year smoker with hypertension and GERD who presented with flank pain and found to have a UTI/pyelonephritis and treated successfully with Cipro. No fevers chills diaphoresis or cough. But he did admit to a 30 pound weight loss without anorexia over about 6 months. A routine CXR showed a nodule: . A CT shown here
. A CT shown here  confirms that. In follow up clinic a month later the CXR looked better:
confirms that. In follow up clinic a month later the CXR looked better: but a CT a month later looked like this:
but a CT a month later looked like this: . What would you do next?
. What would you do next?
After you read the comments, the histology (and answer) can be found here.
70 year old previous 30+ pack year smoker with hypertension and GERD who presented with flank pain and found to have a UTI/pyelonephritis and treated successfully with Cipro. No fevers chills diaphoresis or cough. But he did admit to a 30 pound weight loss without anorexia over about 6 months. A routine CXR showed a nodule:
 . A CT shown here
. A CT shown here  confirms that. In follow up clinic a month later the CXR looked better:
confirms that. In follow up clinic a month later the CXR looked better: but a CT a month later looked like this:
but a CT a month later looked like this: . What would you do next?
. What would you do next?After you read the comments, the histology (and answer) can be found here.
What is active TB?
I will post a case later, but in the meantime, Mike's post on the PPD brings up a good point. What is the radiographic definition of active TB? Is adenopathy active? How about multiple tiny nodules? If you say yes to the latter, how do you know those nodules don't represent non-specific ditzles (like they usually do). If you look up anything on latent vs active, no one (that I could find) actually defines what "active" means. Obviously a cavitary lesion would be one definition, but beyond that it gets very silent out there...
Wednesday, August 24, 2005
Lung abscess?
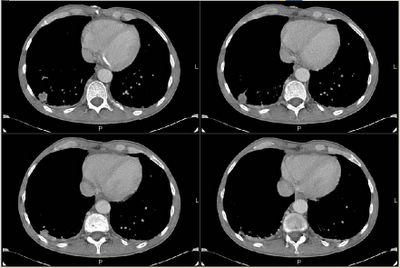
A 74y/o woman was transferred to our institution for her persistent lung abscess. Briefly, she was an otherwise healthy woman until about 5 years ago, when she was diagnosed with a distal esophageal carcinoma, for which she underwent resection with an esophageal pull through and subsequent radiation therapy. Obviously, she did pretty well. About 6 months prior to her current presentation, a LUL nodule was found, and she underwent a left-upper segmentectomy. Following that, she has been seen for a persistent left pleural and pericardial effusions. The etiology of these remained unclear, and she was told it was a "Dressler's type of syndrome."
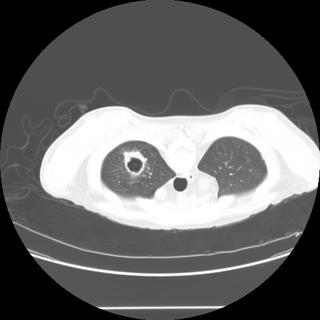
Over a few weeks prior to her transfer, she has developed progressive shortness of breath. No fevers/chills/sweats. No cough or sputum production. No complaints of pain anywhere. She was admitted to another hospital, a chest CT was obtained, and she was transferred to our institution for further management of her lung abscess. Here is a cut from the CT scan done at our institution:

Any comments on the CT scan? Differential diagnosis? Diagnostic studies?
Answer in the comment section below.
Over a few weeks prior to her transfer, she has developed progressive shortness of breath. No fevers/chills/sweats. No cough or sputum production. No complaints of pain anywhere. She was admitted to another hospital, a chest CT was obtained, and she was transferred to our institution for further management of her lung abscess. Here is a cut from the CT scan done at our institution:

Any comments on the CT scan? Differential diagnosis? Diagnostic studies?
Answer in the comment section below.
Tuesday, August 23, 2005
More data on "Abnormal CxR"
Good pick-up on that right sided density. Sorry, I didn't have the lateral view on the computer system so I couldn't post it.
She had a CT of her chest done:
What is your differential now?
Answer in the comment section below.
She had a CT of her chest done:
What is your differential now?
Answer in the comment section below.
Follow-up to "What would you do next?"
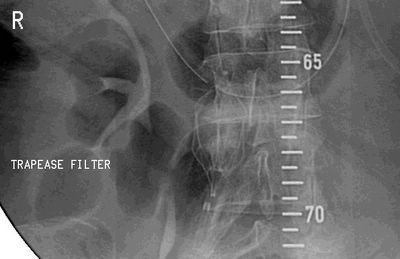
This was the patient with intracranial hemorrhage complicated by saddle embolus.
As everyone pointed out, this was a dificult situation. We had a filter placed:
She had decreased (though still present) radial pulse on the left and we found an occlusive L subclavian/L axillary arterial thrombus with collateral flow.
She developed decreased mentation and though her respiratory status remained the same. She herniated a few nights ago, was made DNR and expired.
As everyone pointed out, this was a dificult situation. We had a filter placed:
She had decreased (though still present) radial pulse on the left and we found an occlusive L subclavian/L axillary arterial thrombus with collateral flow.
She developed decreased mentation and though her respiratory status remained the same. She herniated a few nights ago, was made DNR and expired.
Abnormal CxR
This is a healthy 37 y/o woman who presented to the ER with a cough and had the following chest radiograph:
What is the abnormality? And what is your differential Dx?
Read the comments then see here for a follow-up.
What is the abnormality? And what is your differential Dx?
Read the comments then see here for a follow-up.
Monday, August 22, 2005
Bad looking chest xray
49 year old diagnosed with AML and received chemo 3 weeks ago. As expected he became neutropenic. He received a good many different broad spectrum antibiotics for this neutropenic fever. Three days ago he gradually developed shortness of breath. He remained febrile. His WBC was 9 (up from 4 the day before). At that time his CXR was not remarkable: 
The next day his WBC was 30,k and on the 3rd day it was 45,000. He became more hypoxic. He remained normotensive. His cxr is shown here: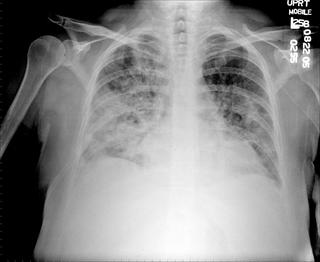
What might be the cause of the CXR findings, in the setting of this presentation?

The next day his WBC was 30,k and on the 3rd day it was 45,000. He became more hypoxic. He remained normotensive. His cxr is shown here:
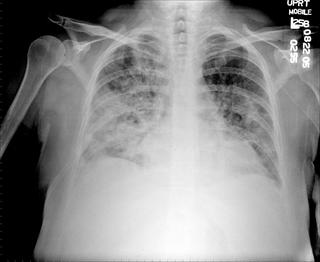
What might be the cause of the CXR findings, in the setting of this presentation?
Friday, August 19, 2005
Effusion - what is the cause?
Question came in today:
"What could be the possible etiology for a pleural effusion that
started after chest pain in a 59 year old; it is exudative, has 480
WBC with 51% PMNs, no micro grew out and the glucose was 183. A
PE-protocol CT was negative. The echo shows normal EF but there is a
small free-flowing pericardial effusion. He had arthoscopic knee
surgery in May but there are no xrays until he came in with CP in
July, where the b/l effusion L>R was found. A CT shpwed bibasilar
airspace disease and atelectasis and the effusion.
How would you put this together, especially with pericardial
involvement. Oh, also he has a high anticardiolipan antibody, but
again, the PE prot CT was negative for PE (and now the effusion is
still there for the past month, and there are no eosinophils in there
either."
"What could be the possible etiology for a pleural effusion that
started after chest pain in a 59 year old; it is exudative, has 480
WBC with 51% PMNs, no micro grew out and the glucose was 183. A
PE-protocol CT was negative. The echo shows normal EF but there is a
small free-flowing pericardial effusion. He had arthoscopic knee
surgery in May but there are no xrays until he came in with CP in
July, where the b/l effusion L>R was found. A CT shpwed bibasilar
airspace disease and atelectasis and the effusion.
How would you put this together, especially with pericardial
involvement. Oh, also he has a high anticardiolipan antibody, but
again, the PE prot CT was negative for PE (and now the effusion is
still there for the past month, and there are no eosinophils in there
either."
Thursday, August 18, 2005
What would you do next?
This has come up today: we have been following this 59 y/o woman on the neurosurgery service. She presented with HTN crisis with a hemorrhagic CVA and has been fairly stable. She has had SCDs on. Tody she had an increase in FiO2 requirements and became more tachycardic. No hypotension. No CP. I got a CT angio that looks as follows.
What would you do next?
The follow-up to this case is posted above on this link.
What would you do next?
The follow-up to this case is posted above on this link.
Paralyzed diaphragm
Here's one from a recent fellow, now out in the real world...
I saw a 57 year old man in Southern Delaware, referred to me for abnormal CT thorax (a pneumatocele). I noticed that his left diaphragm was elevated, and that was not the case on a previous CXR 6 years earlier. Sniff test confirmed left diaphragmatic paralysis. No history of thoracic surgery or trauma. His medical problems includes severe COPD, hypertension and hypercholesterolemia. The CT thorax does not show any masses/tumors. He has emphysematous changes, and calcified granulomas.What is the differential diagnosis and the next step, if any needed?
Thanks for your input.......
.
I saw a 57 year old man in Southern Delaware, referred to me for abnormal CT thorax (a pneumatocele). I noticed that his left diaphragm was elevated, and that was not the case on a previous CXR 6 years earlier. Sniff test confirmed left diaphragmatic paralysis. No history of thoracic surgery or trauma. His medical problems includes severe COPD, hypertension and hypercholesterolemia. The CT thorax does not show any masses/tumors. He has emphysematous changes, and calcified granulomas.What is the differential diagnosis and the next step, if any needed?
Thanks for your input.......
.
Wednesday, August 17, 2005
A case of respiratory failure
Lazar's case:
42 yo male with no significant PMH, family history or tobacco use who was his usual state of health until January of 2005. At that time, he was diagnosed with pneumonia (infiltrate on CXR). He was treated with Biaxin, but developed diarrhea; given a complete course of levofloxacin. He improved to his baseline.
In March of 2005, he noted swelling in multiple joints throughout his body. The most problematic joints included his MCP, wrists, knees, and ankle joints bilaterally. He consulted with a rheumatologist and an extensive laboratory workup was ensued. He was diagnosed with parvovirus B19 and placed on prednisone at 20 mg per day. He remained on prednisone at this dose for roughly one month and was tapered off over the corresponding two weeks.
In early April 2005, the patient again returned to his usual state of health; however in late April, his health worsened again. At that time, he developed Raynaud’s symptoms in his hands with ulcerations on his fingers. A biopsy was performed and he was diagnosed with a nonspecific lymphocytic dermatitis. In late April, he traveled to the Bahamas, and he gradually became more dyspneic. He returned to the continental United States and was referred to an allergist. He was placed on prednisone at 30 mg per day; a diagnosis of asthma made.
In May of 2005, the patient was referred to a pulmonologist. A CT scan of the chest with high resolution cuts was performed; it showed diffuse infiltrates. A bronchoscopy with bronchoalveolar lavage and transbronchial biopsies was performed. This showed a non-specific bronchiolitis. His pulmonologist assumed a diagnosis of BOOP, and increased his prednisone to 70 mg per day.
Over the course of the last two weeks, he developed progressive worsening of shortness of breath. He has a cough with white sputum production in excess of 2 ounces per day.
He presented to the hospital profoundly hypoxemic and was admitted to the MICU on a 100% NRB mask and ultimately was intubated for respiratory failure. He was very hypoxemic and we were unable to oxygenate him (sats were ~ 85% on full paralytics/sedation, inverse ratio, PCV 30 with PEEP 12, FiO2 100%). Bronchoscopy could not be attempted because of his respiratory instability. He had stable hemodynamics, renal function, and hepatic function. His CXR is shown here:
He was ultimately transferred to a major academic center to be evaluated for extracorporeal membrane oxygenation.
42 yo male with no significant PMH, family history or tobacco use who was his usual state of health until January of 2005. At that time, he was diagnosed with pneumonia (infiltrate on CXR). He was treated with Biaxin, but developed diarrhea; given a complete course of levofloxacin. He improved to his baseline.
In March of 2005, he noted swelling in multiple joints throughout his body. The most problematic joints included his MCP, wrists, knees, and ankle joints bilaterally. He consulted with a rheumatologist and an extensive laboratory workup was ensued. He was diagnosed with parvovirus B19 and placed on prednisone at 20 mg per day. He remained on prednisone at this dose for roughly one month and was tapered off over the corresponding two weeks.
In early April 2005, the patient again returned to his usual state of health; however in late April, his health worsened again. At that time, he developed Raynaud’s symptoms in his hands with ulcerations on his fingers. A biopsy was performed and he was diagnosed with a nonspecific lymphocytic dermatitis. In late April, he traveled to the Bahamas, and he gradually became more dyspneic. He returned to the continental United States and was referred to an allergist. He was placed on prednisone at 30 mg per day; a diagnosis of asthma made.
In May of 2005, the patient was referred to a pulmonologist. A CT scan of the chest with high resolution cuts was performed; it showed diffuse infiltrates. A bronchoscopy with bronchoalveolar lavage and transbronchial biopsies was performed. This showed a non-specific bronchiolitis. His pulmonologist assumed a diagnosis of BOOP, and increased his prednisone to 70 mg per day.
Over the course of the last two weeks, he developed progressive worsening of shortness of breath. He has a cough with white sputum production in excess of 2 ounces per day.
He presented to the hospital profoundly hypoxemic and was admitted to the MICU on a 100% NRB mask and ultimately was intubated for respiratory failure. He was very hypoxemic and we were unable to oxygenate him (sats were ~ 85% on full paralytics/sedation, inverse ratio, PCV 30 with PEEP 12, FiO2 100%). Bronchoscopy could not be attempted because of his respiratory instability. He had stable hemodynamics, renal function, and hepatic function. His CXR is shown here:

He was ultimately transferred to a major academic center to be evaluated for extracorporeal membrane oxygenation.
Tuesday, August 16, 2005
Chest pain and abnormal CxR
This is a 52 year-old man. At approximately midnight prio to admission he was eating a piece of chicken on which he choked, gagged and strained and with heavy heaving, he suffered acute onset of abdominal pain and left chest pain. He presented urgently to the hospital and had the following studies.
PMHx: HTN. No previous dysphagia/PUD. No label of pulmonary disease but he smoked 2 ppd. SHx: Occ ETOH, 2 PPD TOB.
ROS: The time from the onset of symptoms to arrival in the ER was approximately 4.5 hours. He has had hematemesis since the onset of the event. He complains of generalized chest pain. No chronic or preceding weight loss or fever or chills, nausea or vomiting or diarrhea.
On exam, he was restless, retching, blood pressure is 154/87, HR is 130. O2 Saturation is 94 to 95%. Chest had crackles and decreased BS at the base. Abdomen was surprisingly benign.
What is your differential and what is the next step?
PMHx: HTN. No previous dysphagia/PUD. No label of pulmonary disease but he smoked 2 ppd. SHx: Occ ETOH, 2 PPD TOB.
ROS: The time from the onset of symptoms to arrival in the ER was approximately 4.5 hours. He has had hematemesis since the onset of the event. He complains of generalized chest pain. No chronic or preceding weight loss or fever or chills, nausea or vomiting or diarrhea.
On exam, he was restless, retching, blood pressure is 154/87, HR is 130. O2 Saturation is 94 to 95%. Chest had crackles and decreased BS at the base. Abdomen was surprisingly benign.
What is your differential and what is the next step?
CT scans added on a new post.
Monday, August 15, 2005
RUL cavitary lesion.
 HC from Michigan has this question: "This gentleman 4 months s/p kidney transplant complaints of shortness of breath. No sputum production. PPD negative pre-transplant. Unable to obtain induced sputums. He had a CT guided biopsy (ID service, before he got to us), of the abnormal finding on CT of the thorax which is negative for AFB and other organisms. Can you reliably rule-out tuberculosis on these grounds without a respiratory sample?; The classic thick vs thin cavity differential diagnosis, can be applied on this case? What is the next step?"
HC from Michigan has this question: "This gentleman 4 months s/p kidney transplant complaints of shortness of breath. No sputum production. PPD negative pre-transplant. Unable to obtain induced sputums. He had a CT guided biopsy (ID service, before he got to us), of the abnormal finding on CT of the thorax which is negative for AFB and other organisms. Can you reliably rule-out tuberculosis on these grounds without a respiratory sample?; The classic thick vs thin cavity differential diagnosis, can be applied on this case? What is the next step?"
Follow up to Friday's chest xray
This is a classic example of collapsed segment of the left lower lobe. You can't usually tell which segment it is, because they will all collapse medially like that and look the same on CXR (because of the pulmonary ligament, it has to collapse that way). The lateral shows some haziness (red circle) and loss of left diaphragm (arrow), but no clear lines to indicate the collapsed lung edge. The PA view clearly shows the collapsed segment (arrows). The CT is shown for comparison.
The patient ended up having an endobronchial lesion at the proximal portion of the left lower lobe. It was squamous cell carcinoma.



The patient ended up having an endobronchial lesion at the proximal portion of the left lower lobe. It was squamous cell carcinoma.

Sunday, August 14, 2005
Question about mometasone
We received this question by email. Any thoughts?
"I am a private practice pulmonologist and was just detailed re: mometasone DPI. The only dose is 220 ug, but it comes in 30, 60 and 120 dose units. The company is telling us that once the DPI is removed from the foil packaging the drug expires in 45 days. This seems to be a ploy to prevent 220 ug QD use with the 120 dose unit, which would be one of the most economical ICS. I searched the web looking data on mometasone stability, and it seems to be a stable molecule. Does anyone know any data? I smell a scam."
"I am a private practice pulmonologist and was just detailed re: mometasone DPI. The only dose is 220 ug, but it comes in 30, 60 and 120 dose units. The company is telling us that once the DPI is removed from the foil packaging the drug expires in 45 days. This seems to be a ploy to prevent 220 ug QD use with the 120 dose unit, which would be one of the most economical ICS. I searched the web looking data on mometasone stability, and it seems to be a stable molecule. Does anyone know any data? I smell a scam."
Friday, August 12, 2005
Friday Radiology - Chest Xray
What is the finding on the chest xray and what is thus the likely diagnosis of this patient? I'll post the chest CT on Monday. Have a good weekend all....


Read the comments and then find the answer Here


Read the comments and then find the answer Here
Follow-up to Wednesday CxR
Good pick-up by Mendez. The CxR has that L for a reason. This is a new patient with Kartagener's who is establishing local pulmonary care. She has chronic sinus disease but not much in the way of bronchiectasis.
COPD and NIPPV
Does anyone know the citation of a study showing an actual survival benefit to using BiPAP ventilation in a patient with a COPD exacerbation vs. conventional mechanical ventilation?
All of the studies listed in Bart Celli's consensus states show trends to survival benefit.
All of the studies listed in Bart Celli's consensus states show trends to survival benefit.
Wednesday, August 10, 2005
Follow-up to ABTx choice
I will wrap this one up so we can focus on JCH's and MLazar's postings.
This is mixed fungal and bacterial endocarditis. Though Candida is a concern and has a fairly high mortality, Aspergillus is the second most common cause of fungal endocarditis and has a very poor prognosis: mortality for treated Aspergillus endocarditis is usually ~80%. The cytology smears were typical of Aspergillus... We started therapy with Vanco (as suggested by JCH I think), gent and Rif (since he had a new prosthetic valve) as well as ampho B and Cancidas. I did not find good data on "double-coverage" for Aspergillu but it has such a dismall prognosis there are many case studies and small series review using Ampho and Voriconazole or Cancidas.
Despite aggressive support his hemodynamics continued to deteriorate for the first week. His family made him a DNR and he died one night of sudden VFib...
This is mixed fungal and bacterial endocarditis. Though Candida is a concern and has a fairly high mortality, Aspergillus is the second most common cause of fungal endocarditis and has a very poor prognosis: mortality for treated Aspergillus endocarditis is usually ~80%. The cytology smears were typical of Aspergillus... We started therapy with Vanco (as suggested by JCH I think), gent and Rif (since he had a new prosthetic valve) as well as ampho B and Cancidas. I did not find good data on "double-coverage" for Aspergillu but it has such a dismall prognosis there are many case studies and small series review using Ampho and Voriconazole or Cancidas.
Despite aggressive support his hemodynamics continued to deteriorate for the first week. His family made him a DNR and he died one night of sudden VFib...
Can we remove this trach
Here's a quick one: 78 y/o man presented to my clinic with the question: can we remove my trach? Actually, he doesn't speak English, and the entire history (or what I could get of one) was provided by his family.
Here's the story: He had a presyncopal episode several months ago and was admitted to another hospital. Developed respiratory distress that night, and was intubated. I have no idea why, but the family says he had been getting narcotics for pain related to the foley (which was placed because he was severely hyperglycemic-known diabetic). Anyway, he self extubated a day later, and required reintubation with 30 minutes. There was apparantly a question of airway edema. A trach was placed 1 week later (no other attempts to remove the tube), and he was discharged to a rehab facility (he was off of the vent).
There, his trach was downsized from an 8 -> 6 -> 4. With the #4, he developed respiratory distress (family things it was a mucous plug). The staff took out the #4, but were unable to get a larger trach in, so he was orally intubated again. A repeat trach was placed 2 days later, and he was in the ICU for 3 weeks (again, I get no history of a pneumonia or mechanical respiratory failure, but I'm told he was on the vent for most of that time) prior to transfer back to rehab.
He was in rehab for 2 months, and now home for 1 month. He's got an uncuffed 6-shiley and caps it without difficulty. He's got a Passey-Muir that he uses to speak with family.
Only other PMH is multi-infart dementia. The rest of the history and exam are unremarkable. Spirometry shows a fixed obstruction-classic-if anyone wants it for their teaching files, let me know.
Anyway, what do you tell them? Can we decannulate?
Here's the story: He had a presyncopal episode several months ago and was admitted to another hospital. Developed respiratory distress that night, and was intubated. I have no idea why, but the family says he had been getting narcotics for pain related to the foley (which was placed because he was severely hyperglycemic-known diabetic). Anyway, he self extubated a day later, and required reintubation with 30 minutes. There was apparantly a question of airway edema. A trach was placed 1 week later (no other attempts to remove the tube), and he was discharged to a rehab facility (he was off of the vent).
There, his trach was downsized from an 8 -> 6 -> 4. With the #4, he developed respiratory distress (family things it was a mucous plug). The staff took out the #4, but were unable to get a larger trach in, so he was orally intubated again. A repeat trach was placed 2 days later, and he was in the ICU for 3 weeks (again, I get no history of a pneumonia or mechanical respiratory failure, but I'm told he was on the vent for most of that time) prior to transfer back to rehab.
He was in rehab for 2 months, and now home for 1 month. He's got an uncuffed 6-shiley and caps it without difficulty. He's got a Passey-Muir that he uses to speak with family.
Only other PMH is multi-infart dementia. The rest of the history and exam are unremarkable. Spirometry shows a fixed obstruction-classic-if anyone wants it for their teaching files, let me know.
Anyway, what do you tell them? Can we decannulate?
Dypnea with a pleural effusion
81 yo male with a past history of obstructive jaundice s/p ERCP and removal of a stone one week prior to readmission. He was discharged from the hospital shortly after this procedure at which he was returned to his care facility for two to three weeks. While at his NH, he started to have worsening shortness of breath which has worsened over the last 2 months but has become more profound in the last week. It is worse with exertion and he can currently only walk approximately 10 feet. He denies any complaints of chest pain, calf pain or calf swelling. He has no history of venous thromboembolic disease. The patient denies wheezing, cough or sputum production, hemoptysis, a runny nose, reflux symptoms or palpitations.
PAST MEDICAL HISTORY: Obstructive jaundice secondary to gallstones; COPD per his PCP's records.
SOCIAL HISTORY: Smoking history: 20 pack years; he quit 15 years ago.
Alcohol use: The patient admits to 6 to 7 beers per week for approximately 60 years.
He denies IV or street drug use. He was exposed to asbestos for approximately 7 months as he was working in a factory in which the asbestos was being removed. No travel.
PE: Vitals: Heart rate 76, resps 18. BP 136/76. Saturation: 96% on Room Air. Neck: No JVD. Heart: Normal. Lungs: clear throughout all fields, however, decreased BS in all fields. Extremities: Fingernails positive for clubbing. Pitting edema noted in the lower extremities.
Labs: Sodium 142, potassium 4.3, chloride 110, bicarb 23, BUN 6, creatinine 1.0, glucose 98, calcium 8.2, phosphorus 2.7, albumin 2.3, total protein 5.0, alk phos 151, AST 26, ALT 38, total bili 3.5, direct bili 1.8.
white blood cells 8.6, H and H 9.4, and 29.7 platelets 771.
RADIOGRAPHS:



How would you proceed? What tests would you want next?
PAST MEDICAL HISTORY: Obstructive jaundice secondary to gallstones; COPD per his PCP's records.
SOCIAL HISTORY: Smoking history: 20 pack years; he quit 15 years ago.
Alcohol use: The patient admits to 6 to 7 beers per week for approximately 60 years.
He denies IV or street drug use. He was exposed to asbestos for approximately 7 months as he was working in a factory in which the asbestos was being removed. No travel.
PE: Vitals: Heart rate 76, resps 18. BP 136/76. Saturation: 96% on Room Air. Neck: No JVD. Heart: Normal. Lungs: clear throughout all fields, however, decreased BS in all fields. Extremities: Fingernails positive for clubbing. Pitting edema noted in the lower extremities.
Labs: Sodium 142, potassium 4.3, chloride 110, bicarb 23, BUN 6, creatinine 1.0, glucose 98, calcium 8.2, phosphorus 2.7, albumin 2.3, total protein 5.0, alk phos 151, AST 26, ALT 38, total bili 3.5, direct bili 1.8.
white blood cells 8.6, H and H 9.4, and 29.7 platelets 771.
RADIOGRAPHS:



How would you proceed? What tests would you want next?
New ICS
Has anybody used or had any experience with the new mometasone inhaler (Asmanex)?
It comes in an auto-haler similar to Pulmicort but it has a counter which is a nice improvement over Pulmicort.
It comes in an auto-haler similar to Pulmicort but it has a counter which is a nice improvement over Pulmicort.
Tuesday, August 09, 2005
Just a quick question while we are all mulling over Carlos' post; if a patient had resection of some RUL aspergilloma and he is going to get a renal transplant (thus immunosuppressed), do you give that patient prophylactic itraconazole after the kidney transplant?
Choices of ABTx
We were consulted to see this is 72-year-old man following emergent aortic valve replacement. He had had a CABG in 2000 and ha done extremely well until approximately two to three weeks PTA when he began experiencing increasing shortness of breath and dyspnea on exertionre. He was seen by cardiology and a 2-D-ECHO revealed aortic insufficiency and possible signs of Valsalva to left atrial fistula. He had an emergent valve replacement and we were consulted because the valve appeared grossly infected and intra-op swabs revealed GPCs in chains and yeast on smears.
He was intubated and on pressors post-op. What would you like to know and what ABTx would you recommend?
He was intubated and on pressors post-op. What would you like to know and what ABTx would you recommend?
Follow-up to hypercalcemia
This is the 61 y/o man with a pulmonary mass and the bony lesions that Jennings astutely thought looked like a plasmacytoma. I was also impressed by the combination of lung mass and hypercalcemia. There were no other thoracic lesions.
We started standard hyperCa++ treatment, his MS improved and his creatinine came down from 2.0 to o.8 with normalization of his Ca++.
We set him up for a CT-guided Bx of his lung mass: he developed massive hemoptysis, almost coded; we emergently intubated him and I used the bronchoscope to advance the ETT towards a selective L intubation...
He recovered and prior to re-Bx'ing we repeated a CT scan and the nodule was gone!
He went home to recover from his respiratory failure and we finished his w/up as an outpatient: no more lung masses but his bone lesions and BM Bx led to a diagnosis of multiple myeloma.
We started standard hyperCa++ treatment, his MS improved and his creatinine came down from 2.0 to o.8 with normalization of his Ca++.
We set him up for a CT-guided Bx of his lung mass: he developed massive hemoptysis, almost coded; we emergently intubated him and I used the bronchoscope to advance the ETT towards a selective L intubation...
He recovered and prior to re-Bx'ing we repeated a CT scan and the nodule was gone!
He went home to recover from his respiratory failure and we finished his w/up as an outpatient: no more lung masses but his bone lesions and BM Bx led to a diagnosis of multiple myeloma.
Monday, August 08, 2005
Friday, August 05, 2005
DVT and ambulation
Here's another interesting question we received:
"Hello. Great blog. We have a patient with an extensive DVT. He is being heparinised. He asked if he should walk on it. Is there a risk of embolization events if you walk on a leg with DVT? If so, what is the time frame in which it becomes safe to do so? On the other hand, is it better or worse to keep the leg up and stay in bed? This would seem counterintuitive to virchow's triad which warns agains immobilisation."
"Hello. Great blog. We have a patient with an extensive DVT. He is being heparinised. He asked if he should walk on it. Is there a risk of embolization events if you walk on a leg with DVT? If so, what is the time frame in which it becomes safe to do so? On the other hand, is it better or worse to keep the leg up and stay in bed? This would seem counterintuitive to virchow's triad which warns agains immobilisation."
Airborn
A 3rd year resident had an interesting question. He wanted to see what others thought. He asks, "we are all taught that bacterial pneumonia is not 'catching'. You can put a patient with community-acquired pneumonia, i.e. strep pneumonia, in the same room as someone else and their roommate will not catch pneumonia. Why then is TB contagious, when this is ALSO a bacteria? Or to put it another way, why is TB the only type of bacterial pneumonia that is contagious?"
Wednesday, August 03, 2005
Hypercalcemia and lung mass
This is a 61 y/o man with a significant Hx of smoking. He presented to our ER with a 3-week history of polyuria, weakness, fatigue, confusion and abdominal pain. Using my keen diagnostic skills I asked the ER to check a calcium level which was 15.2. He was admitted and treated for the hypercalcemia.
His Cxr showed some hyperinflation and a RLL pulmonary nodule better characterized on the CT scan below (check out the vertebral bodies).
What would you do next? What is your differential?
His Cxr showed some hyperinflation and a RLL pulmonary nodule better characterized on the CT scan below (check out the vertebral bodies).
What would you do next? What is your differential?
Answer/follow-up to this case on http://pulmonaryroundtable.blogspot.com/2005/08/follow-up-to-hypercalcemia.html
Tuesday, August 02, 2005
CT followup?
This question is from a doc in Ohio:
A f/u CT was done on a patient 1 and 1/2 months after RUL community-aquired pneumonia.
The reading was: "Small focal pneumonic process in the anterior subsegment of the right upper lobe. The 2 tiny nodules in the right lower lobe likely represent
noncalcified granulomas or intrapulmonary lymph nodes."
Does this patient need any more f/u CT's based on thsi interpretation?
A f/u CT was done on a patient 1 and 1/2 months after RUL community-aquired pneumonia.
The reading was: "Small focal pneumonic process in the anterior subsegment of the right upper lobe. The 2 tiny nodules in the right lower lobe likely represent
noncalcified granulomas or intrapulmonary lymph nodes."
Does this patient need any more f/u CT's based on thsi interpretation?
Monday, August 01, 2005
CT for back pain
Subscribe to:
Posts (Atom)