This was submitted to us:
34yr.old female w/ previous rt low lobe nodules since 2001 CT revealed the nodules while patient had chickenpox.
New CT in 2006 shows new node on lt. upper diaphragm. Last CT 6mo. prior didnt show nodule, which is uncalcified unlike rt. lung nodes.
PT. has nightsweats wt. loss chronic pelvic abdominal pain jointpain/swell/stiff no appetite ab.bloat chronic urinary symptoms and UTI.
Now with SWOLLENLYMPHNODES W/LYMPH SURFACING AND RUPTURE ON NECK BACK OF HEAD BEHIND EAR. PT. is 11/2 ppd smoker of 13yrs. PET done 4/06 and no malignant chest activity. labs almost normal.
Monday, August 14, 2006
Wedding bells
Congratulations to one of our editors: Jeff Jennings tied the knot this past weekend.
We will keep posting while he is on his honeymoon.
We will keep posting while he is on his honeymoon.
Wednesday, August 09, 2006
Acid Base
The chem-7 and the gas were both drawn within 22 minutes of each other in this 71 year old intubated man with sepsis and ARDS:
7.08/24/226 on fio2 of 75%
Na 145
k 5.2
Cl- 114
HCO3 28
BUN 42
Cr 0.5
What is the acid base disturbance?
7.08/24/226 on fio2 of 75%
Na 145
k 5.2
Cl- 114
HCO3 28
BUN 42
Cr 0.5
What is the acid base disturbance?
Proceed or watch? Is it CA?
Here is a case submitted to us:
8/1/06 49 YO Caucasion male, married with minor children, comfortably employed professional, USAF Gulf War Veteran, 2-3 PPD smoker X30 years, ETOH dependent (averages 6-10 beers daily)presents with R clavicular pain after home remodeling project. Well developed, well nourished, muscular, athletic body type. VS WNL. Non remarkable EKG. Clavicle XR demonstrates shoulder separation with incidental 1.75cm diameter spiculated nodule mid upper right lobe lung, mild emphysematous changes. CT confirms nodule. PET eyes to knees results no demonstrative uptakes. CBC, Metabolic panels normal. CEA and CA125 WNL. PFTs near normal, demonstrates ability to tolerate surgery.
Family HX: Maternal died d/t +NSCL CA with brain, liver mets. Paternal +adenocarcinoma colon, in remission post colectomy and chemo. No other significant family HX or disease.
Smoking Cessation in process with nicotine patch use. ETOH use diminishing. Pt. wants no invasive surgery or BX unless absolutely indicated. Lesion is not near bronch, no bronchoscopy in plan. What next?
8/1/06 49 YO Caucasion male, married with minor children, comfortably employed professional, USAF Gulf War Veteran, 2-3 PPD smoker X30 years, ETOH dependent (averages 6-10 beers daily)presents with R clavicular pain after home remodeling project. Well developed, well nourished, muscular, athletic body type. VS WNL. Non remarkable EKG. Clavicle XR demonstrates shoulder separation with incidental 1.75cm diameter spiculated nodule mid upper right lobe lung, mild emphysematous changes. CT confirms nodule. PET eyes to knees results no demonstrative uptakes. CBC, Metabolic panels normal. CEA and CA125 WNL. PFTs near normal, demonstrates ability to tolerate surgery.
Family HX: Maternal died d/t +NSCL CA with brain, liver mets. Paternal +adenocarcinoma colon, in remission post colectomy and chemo. No other significant family HX or disease.
Smoking Cessation in process with nicotine patch use. ETOH use diminishing. Pt. wants no invasive surgery or BX unless absolutely indicated. Lesion is not near bronch, no bronchoscopy in plan. What next?
Tuesday, August 08, 2006
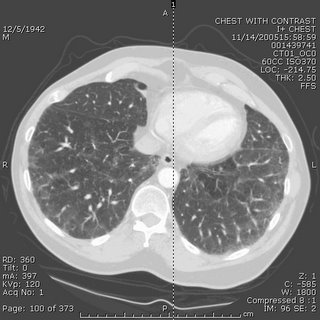
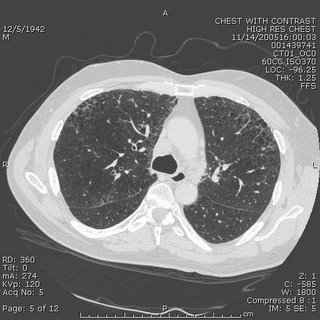
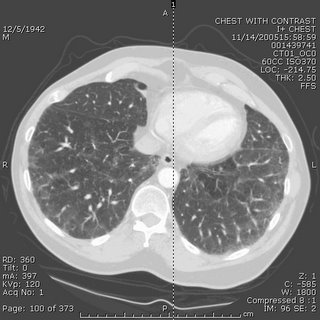
Mass and infiltrates
This is a 59 y/o woman with a funny presentation: she had an episode of syncope at home, hit her head and had a skin lac requiring 7 stitches. While being worked up in the ER they found her to be hypotensive and febrile with an abnormal CxR and CT of the chest. She had MSSA in her sputum and the dense "mass" seen on the left images. I bronch'ed her and got "organizing pneumonia" but no malignancy. She got ABTx and the "mass" went away completely.
She has felt better and has good PFTs. However, it has now been 3 months and the peripheral faint patchy areas of reticular disease remain there and unchanged.
She has only minimal DOE. She quit smoking in 1988 and has no unusual exposures.
How would you pursue this little infiltrates? (they are present in the lower lobes as well).

She has felt better and has good PFTs. However, it has now been 3 months and the peripheral faint patchy areas of reticular disease remain there and unchanged.
She has only minimal DOE. She quit smoking in 1988 and has no unusual exposures.
How would you pursue this little infiltrates? (they are present in the lower lobes as well).

Thursday, August 03, 2006
Halleliujah
From Arenberg:
"In celebration of the fact that the IT people in the Department of Radiology at the University of of Michigan have recognozed that their department exists to provide films for other doctors to look at, and have finally made it into the 21st centry by providing consistent, relaible online access to films for the unwashed masses (read: non-radiologists)...I hereby submit this film of an unfortunate man with a history of cancer."

"In celebration of the fact that the IT people in the Department of Radiology at the University of of Michigan have recognozed that their department exists to provide films for other doctors to look at, and have finally made it into the 21st centry by providing consistent, relaible online access to films for the unwashed masses (read: non-radiologists)...I hereby submit this film of an unfortunate man with a history of cancer."

Monday, July 31, 2006
Follow up to pleuritic pain and fatigue
Old case presented by Mendez is here.
Follow up: Transbronchial bx's revealed multiple epithelioid granulomas. Special stains for AFB and fungi were negative.
Symptoms improved after treatment with oral prednisone which was tapered over several months.
F/U Chest CT (6 months later) revealed interval regression of peribronchovascular nodularity. Previously enlarged hilar/mediastinal lymph nodes no longer enlarged.
Final Dx: Stage II Sarcoid
Follow up: Transbronchial bx's revealed multiple epithelioid granulomas. Special stains for AFB and fungi were negative.
Symptoms improved after treatment with oral prednisone which was tapered over several months.
F/U Chest CT (6 months later) revealed interval regression of peribronchovascular nodularity. Previously enlarged hilar/mediastinal lymph nodes no longer enlarged.
Final Dx: Stage II Sarcoid
Sunday, July 30, 2006
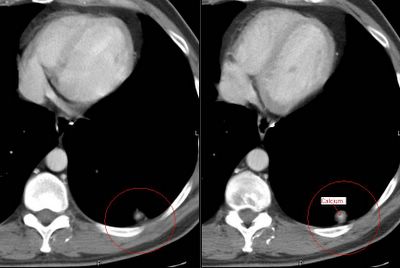
Pulmonary nodules
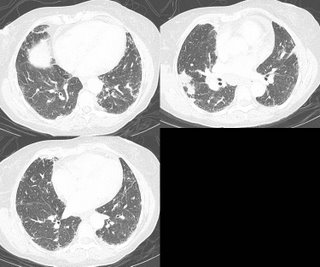
This is a 44 y/o man who works here in the hospital. He is a ctually a nice guy so I'm trying not to find anything too interesting on his case.
He is very healthy and smoked a pack-a-day for ten years but quit in 1988. He had travelled to the gul area and came back with a severe gastroenteritis. It seems that it was so bad the primary team got a CT of his abdomen. He did OK but the lower cuts of the lung revealed a ~1-cm partially calcified LLL nodule. He is completely asymptomatic from a respiratory perspective. His PFTs are completely normal. We got a dedicated CT of the chest and found the following nodules: (a 9-mm RUL a ~5-mm L apical and the same LLL).
The RUL has a little bit of excentric calcium as does the LLL one. Would you PET, biopsy, watch or else?
He is very healthy and smoked a pack-a-day for ten years but quit in 1988. He had travelled to the gul area and came back with a severe gastroenteritis. It seems that it was so bad the primary team got a CT of his abdomen. He did OK but the lower cuts of the lung revealed a ~1-cm partially calcified LLL nodule. He is completely asymptomatic from a respiratory perspective. His PFTs are completely normal. We got a dedicated CT of the chest and found the following nodules: (a 9-mm RUL a ~5-mm L apical and the same LLL).
The RUL has a little bit of excentric calcium as does the LLL one. Would you PET, biopsy, watch or else?
Thursday, July 27, 2006
mediastinal nodes
Case submitted from outside:
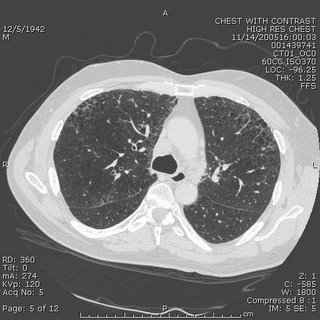
63 year old smoker with hypoxia. CXR looks extremely hyperinflated. PFTs with ratio of 0.67, FEV1 87% predicted and FVC 93%. Lung volumes normal except for an inspiratory capacity of 73% predicted (volume done by helium dilution). DLCO 35% predicted. CT scans included below and are basically unchanged from 7 months ago. Mild mediastinal LAD, with the largest being approx 2cm. Also stable over 7 months. Would anyone pursue a biopsy of the nodes or the lung? Other thoughts?



63 year old smoker with hypoxia. CXR looks extremely hyperinflated. PFTs with ratio of 0.67, FEV1 87% predicted and FVC 93%. Lung volumes normal except for an inspiratory capacity of 73% predicted (volume done by helium dilution). DLCO 35% predicted. CT scans included below and are basically unchanged from 7 months ago. Mild mediastinal LAD, with the largest being approx 2cm. Also stable over 7 months. Would anyone pursue a biopsy of the nodes or the lung? Other thoughts?



Wednesday, July 26, 2006
LVRS contra-indication
This question came up recently on this patient's follow-up. This is a relatively young man with HIV/AIDS who has done remarkably well on HAART (he had PCP 8 years ago!). He has the typical bullous emphysema associated with HIV and his previous smoking history. His emphysema is predominantly upper lobe (see below with a nice azygous "lobe"), he is hyperinflated and has air trapping. His FEV1 is still greater than 45% so LVRS is not for him yet anyway.
However, the question came up, is HIV infection an absolute contra-indication to LVRS?
However, the question came up, is HIV infection an absolute contra-indication to LVRS?
Tuesday, July 25, 2006
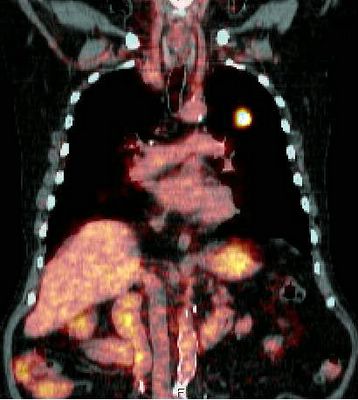
New lung nodule
This is a 72 y/o man with a significant previous TOB Hx, moderate COPD who was referred to us for a new pulmonary nodule. He has had multiple urologic surgeries including a nephrectomy for transitional cell ca (it seems he had a "high" transitional ca of the calicial system). He has a new nodule on the contra-lateral (remaining) kidney and had a new CT and a pulmonary nodule was found. This is a LUL non-calcified nodule with no air-space disease and no thoracic adenopathy.
A bronch was non-diagnostic and a PET (see below) only showed intense uptake on the nodule and nowhere else (the remaining kidney had its usual physiologic uptake).
Do you think the two lesions are related? Would you try and FNA the lesion? His PFTs would tolerate a lobectomy. Would you just go straight to surgery?
A bronch was non-diagnostic and a PET (see below) only showed intense uptake on the nodule and nowhere else (the remaining kidney had its usual physiologic uptake).
Do you think the two lesions are related? Would you try and FNA the lesion? His PFTs would tolerate a lobectomy. Would you just go straight to surgery?
Monday, July 24, 2006
More on the woman with eosinophilia
Well, as you might remember, this patient with a past medical history of asthma had had a few months of dyspnea and malaise. A peripheral showed 42% eosinophils and a BAL showed 20% eosinophils. A transbronchial biopsy showed eosinophilic infiltration. Micro was negative. Stool O&P was also negative.
She was given steroids with subjective improvement. However, I am not entirely satisfied with a diagnosis of chronic eosinophilic pneumonia. Here are her radiographs:

Now her amylase and lipase are elevated which does not go with eosinophilic pneumonia, and I don't have a good reason for that. Any thoughts out there? If it is parasitic, at least she is not worsening on the steroids....
She was given steroids with subjective improvement. However, I am not entirely satisfied with a diagnosis of chronic eosinophilic pneumonia. Here are her radiographs:

Now her amylase and lipase are elevated which does not go with eosinophilic pneumonia, and I don't have a good reason for that. Any thoughts out there? If it is parasitic, at least she is not worsening on the steroids....
Thursday, July 20, 2006
AAT replacement
Question came in from here:
Just a quick question on alfa-1 antitrypsin replacement.
Do you use weekly regimen or monthly regimen? FDA has approved only once a week regimen. But I have read that monthly regimen is also "widely used in many centers." What is your experience on this? Monthly regimen would be off-label use. Has anybody experienced a severe adverse effect with monthly regimen?
Just a quick question on alfa-1 antitrypsin replacement.
Do you use weekly regimen or monthly regimen? FDA has approved only once a week regimen. But I have read that monthly regimen is also "widely used in many centers." What is your experience on this? Monthly regimen would be off-label use. Has anybody experienced a severe adverse effect with monthly regimen?
Radiation and lung cancer
I think it is my week to pick on radiation Tx... I already posted on the time delay notion (BTW, check out the PPT on that listed on the comments section).
What is your impression/practice on the use of xRt and lung cancer?
It certainly has an excellent role in symptom palliation, particularly with painful bony mets and other solitary mets presentations. It does decrease local recurrence (though it has less of an impact on survival) in locally advanced disease but it seems to me that it is automatically lumped with chemo as if you must have one with the other.
As a single modality (“curative xRt”) kind of falls short:
In a review of ten studies that utilized megavoltage irradiation to doses of >55 gray (Gy) in conventional fractionation for patients with medically inoperable Stage I lung carcinoma, only approximately 15% of patients were long term survivors (vs surgery and multimodality Tx). Cancer 1998 Feb 1;82(3):433-8
Similarly, five-year survival was only 19 percent in a series of "medically inoperable" patients with stage II disease. Radiat Oncol Invest 1996; 4:165
And the data on post-op xRt is not as good as post-op chemo:
In a French trial of post-op xRt vs. observation only, five-year overall survival was 43% for the control group and 30% for the radiotherapy group (P = 0.002). Cancer 1999 Jul 15;86(2):265-73
The older Lung Cancer Study Group from 86 showed no evidence that radiotherapy improved survival, and although recurrence rates appeared to be somewhat reduced among patients assigned to radiotherapy, these decreases were not statistically significant. N Engl J Med 1986 Nov 27;315(22):1377-81
In the IALT trial, which focused on post-op therapy and showed a benefit for chemo,
only 70.4 percent of those assigned to receive adjuvant thoracic radiotherapy in the chemotherapy group actually received xRt and the control group had actually a higher rate of xRt. N Engl J Med 2004 Jan 22;350(4):351-60
The PORT meta-analysis even showed a significant adverse effect of postoperative radiotherapy on survival (hazard ratio 1.21 [95% CI 1.08-1.34]). Lancet. 1998 Jul 25;352(9124):257-63
Even in stage III dz, whether they have N2 dz or a T4 things are not that clear:
Patients with non-small cell lung cancer who had inoperable, nonmetastatic disease gained no clinically meaningful survival advantage with immediate thoracic irradiation, even when modern megavoltage radiation therapy techniques and equipment was used in Ann Intern Med 1990 Jul 1;113(1):33-8. And in minimally symptomatic patients with locally advanced non-small cell lung cancer, “no persuasive evidence was found to indicate that giving immediate palliative thoracic radiotherapy improves symptom control, quality of life, or survival when compared with delaying until symptoms require treatment”. BMJ 2002 Aug 31;325(7362):465
What do you think?
What is your impression/practice on the use of xRt and lung cancer?
It certainly has an excellent role in symptom palliation, particularly with painful bony mets and other solitary mets presentations. It does decrease local recurrence (though it has less of an impact on survival) in locally advanced disease but it seems to me that it is automatically lumped with chemo as if you must have one with the other.
As a single modality (“curative xRt”) kind of falls short:
In a review of ten studies that utilized megavoltage irradiation to doses of >55 gray (Gy) in conventional fractionation for patients with medically inoperable Stage I lung carcinoma, only approximately 15% of patients were long term survivors (vs surgery and multimodality Tx). Cancer 1998 Feb 1;82(3):433-8
Similarly, five-year survival was only 19 percent in a series of "medically inoperable" patients with stage II disease. Radiat Oncol Invest 1996; 4:165
And the data on post-op xRt is not as good as post-op chemo:
In a French trial of post-op xRt vs. observation only, five-year overall survival was 43% for the control group and 30% for the radiotherapy group (P = 0.002). Cancer 1999 Jul 15;86(2):265-73
The older Lung Cancer Study Group from 86 showed no evidence that radiotherapy improved survival, and although recurrence rates appeared to be somewhat reduced among patients assigned to radiotherapy, these decreases were not statistically significant. N Engl J Med 1986 Nov 27;315(22):1377-81
In the IALT trial, which focused on post-op therapy and showed a benefit for chemo,
only 70.4 percent of those assigned to receive adjuvant thoracic radiotherapy in the chemotherapy group actually received xRt and the control group had actually a higher rate of xRt. N Engl J Med 2004 Jan 22;350(4):351-60
The PORT meta-analysis even showed a significant adverse effect of postoperative radiotherapy on survival (hazard ratio 1.21 [95% CI 1.08-1.34]). Lancet. 1998 Jul 25;352(9124):257-63
Even in stage III dz, whether they have N2 dz or a T4 things are not that clear:
Patients with non-small cell lung cancer who had inoperable, nonmetastatic disease gained no clinically meaningful survival advantage with immediate thoracic irradiation, even when modern megavoltage radiation therapy techniques and equipment was used in Ann Intern Med 1990 Jul 1;113(1):33-8. And in minimally symptomatic patients with locally advanced non-small cell lung cancer, “no persuasive evidence was found to indicate that giving immediate palliative thoracic radiotherapy improves symptom control, quality of life, or survival when compared with delaying until symptoms require treatment”. BMJ 2002 Aug 31;325(7362):465
What do you think?
Tuesday, July 18, 2006
Here's one from the "huh" category
In a letter I received today, summarizing a patient's recent hospitalization:
"...led us to the decision that a below-elbow amputation would help us to decrease her morbidity and would not eliminate any significant hand function."
I can't think of many things that would eliminate significant hand function MORE than a below-elbow amputation. But hey, I'm just a lung doc...
"...led us to the decision that a below-elbow amputation would help us to decrease her morbidity and would not eliminate any significant hand function."
I can't think of many things that would eliminate significant hand function MORE than a below-elbow amputation. But hey, I'm just a lung doc...
Time to Chemo and xRt
This has come up in discussions with our hem-onc dept.: Hem-onc has been frustrated by perceived delays from "first abnormal CxRay" to "definitive treatment". Our position is that diagnostic eval should be quick to try and identify possible surgical candidates and that 1-2 weeks (or even a bit more if they do get surgery) added on by staging and diagnostic procedures would not impact response to Chemo/xRt much. Other than perhaps the more aggressive small-cell case, chemo and xRt are usually either adjuvant or reverved for more advanced stages.
Do you know of actual data looking at time from diagnosis to chemo and impact on outcomes?
Do you know of actual data looking at time from diagnosis to chemo and impact on outcomes?
Obesity and lung disease
I had posted on obesity and obstructive lung disease but did not get much feedback...
JJ had an interesting aside on BMI progression over time.
Anybody (Lazar?) went to the ATS section on obesity and lung Dz? Any other insight on obstructive ventilatory defects, RAD and obesity?
JJ had an interesting aside on BMI progression over time.
Anybody (Lazar?) went to the ATS section on obesity and lung Dz? Any other insight on obstructive ventilatory defects, RAD and obesity?
Smoking cessation
JJ had posted on the JAMA article on Varenicline (Pfizer's Chantix for smoking cessation).
Has anybody had a chance to prescribe it yet?
There is a reported fairly high rate of nausea but it is also reported to be mild and transient. Any experience with that?
Has anybody had a chance to prescribe it yet?
There is a reported fairly high rate of nausea but it is also reported to be mild and transient. Any experience with that?
Monday, July 17, 2006
TBBx protocol
AK asks:
Wondering how many people out there do blind TBB's or if fluoro is pretty routine. Do people favor a particular protocol? I've seen people try to have the patient exhale, others just check if the forceps cause pain then let her rip. Would be curious to hear different techniques used out there.
Wondering how many people out there do blind TBB's or if fluoro is pretty routine. Do people favor a particular protocol? I've seen people try to have the patient exhale, others just check if the forceps cause pain then let her rip. Would be curious to hear different techniques used out there.
Friday, July 14, 2006
56 year old woman with eosinophilia
56-year-old woman with a past medical history of asthma since age 38 with 2 previous courses of steroids, otherwise well controlled who presented with increase in non-productive cough and really very minimal SOB except on exertion. A cxr revealed b/l upper lobe infiltrates. She denies any hemoptysis and has lost about 14 pounds. She initially began her evaluation for this disease process in May 06 by ID. Her appetite is poor.


A CBC showed a white count of 17 with 42% eosinophils.
A BAL showed a cell count of 696 with 20% eosinophils, 40% macrophages, 11% lymphocytes.
A TBBX showed: Active lung injury with eosinophilia. 2. Grocott stain is negative for fungus
Based on this, the pathologist thought the ddx (which is close to mine before I saw the bx results): Diagnostic considerations include acute eosinophilic pneumonia, which is favored, an underlying infectious etiology, and Churg-Strauss syndrome/
Wegener's granulomatosis. Microbiologic and serologic studies would allow for
exclusion of the latter choices.
I would also add ABPA to that list.
Of note, the BAL was negative for all micro.
Now, my question is, would you treat this patient with steroids, since nearly everyhting on that list is trreatable with steroids, or would you proceed to open lung for a definitive dx? The reason for the latter is that even though these disease are all similarly treated, their prognosis and natural courses are different and this would be helpful for future care.
What are your thoughts?


A CBC showed a white count of 17 with 42% eosinophils.
A BAL showed a cell count of 696 with 20% eosinophils, 40% macrophages, 11% lymphocytes.
A TBBX showed: Active lung injury with eosinophilia. 2. Grocott stain is negative for fungus
Based on this, the pathologist thought the ddx (which is close to mine before I saw the bx results): Diagnostic considerations include acute eosinophilic pneumonia, which is favored, an underlying infectious etiology, and Churg-Strauss syndrome/
Wegener's granulomatosis. Microbiologic and serologic studies would allow for
exclusion of the latter choices.
I would also add ABPA to that list.
Of note, the BAL was negative for all micro.
Now, my question is, would you treat this patient with steroids, since nearly everyhting on that list is trreatable with steroids, or would you proceed to open lung for a definitive dx? The reason for the latter is that even though these disease are all similarly treated, their prognosis and natural courses are different and this would be helpful for future care.
What are your thoughts?
Subscribe to:
Posts (Atom)