

A CBC showed a white count of 17 with 42% eosinophils.
A BAL showed a cell count of 696 with 20% eosinophils, 40% macrophages, 11% lymphocytes.
A TBBX showed: Active lung injury with eosinophilia. 2. Grocott stain is negative for fungus
Based on this, the pathologist thought the ddx (which is close to mine before I saw the bx results): Diagnostic considerations include acute eosinophilic pneumonia, which is favored, an underlying infectious etiology, and Churg-Strauss syndrome/
Wegener's granulomatosis. Microbiologic and serologic studies would allow for
exclusion of the latter choices.
I would also add ABPA to that list.
Of note, the BAL was negative for all micro.
Now, my question is, would you treat this patient with steroids, since nearly everyhting on that list is trreatable with steroids, or would you proceed to open lung for a definitive dx? The reason for the latter is that even though these disease are all similarly treated, their prognosis and natural courses are different and this would be helpful for future care.
What are your thoughts?
4 comments - CLICK HERE to read & add your own!:
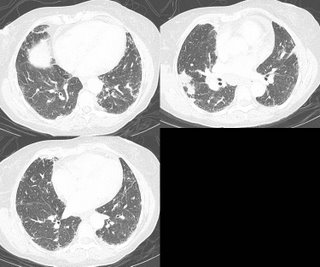
I agree--even the pattern on CT, with more peripheral infiltrates, is consistent with chronic eosinophilic pneumonia.
The liklihood of Wegener's here seems pretty low, and I'd accept a negative C-ANCA and a bland urine microscopy as excluding it. There is no bronciectasis, which would be more likely with ABPA or churg-strauss, and "asthma" symptoms don't seem to be a prominent feature of her current presentation. Additionally, you havn't described any sinus-related symptoms, which could be associated with those diagnoses. Biopsy had no evidence of vasculitis, although a TBBX is not definitive. Moreover, these are less likely to have profound eosinophilia on the BAL.
I forgot to add a very important thing: she presented to the hospital with nausea, vomiting and mild, loose sttols/diarrhea. She cannot tolerate PO's. We sent the O&P, ANCA's, IgE as suggested.
The multiple courses of steroids may falsely lower Mendez's IgE level. A RAST against aspergillus would be helpful, but at Beaumont, it is much easier to get serum precipitans to AF. I am not sure what is easier at U of M or HFH.
Agreed with CEP as the diagnosis (again, assuming JCH's urine is without RBC's and the ANCA is negative).
Follow-up seen here:
http://pulmonaryroundtable.blogspot.com/2006/07/more-on-woman-with-eosinophilia.html
Post a Commenttest post a comment