Her hospital course was complicated by VDRF requiring about 2 weeks on the vent. A BAL of her LLL was performed and yielded (per her report) "Valley Fever." She was placed on fluconazole (unknown dose). Her chest xray showed lobar pneumonia. PPD negative at OSH; BAL neg for AFB.
She slowly recovered and presented to my office 8 months later with dyspnea, fatigue and chest pain. She was being treated with Fluconazole 100 mg daily and had been on that dose for the last few months.
Her chest pain was typical for cardiac, so I got a functional study of her heart. It was positive. A cath was performed by cardiology and a PTCA/stent was placed in her PDA; her symptoms clearly improved. However, she was not back at her baseline.
PMH: CAD, Thoracic Aortic aneurysm (stable x 4 years), HTN, hyperlipidemia, obesity (182 lbs; 5"3')
SH: no tob, etoh, drugs, travel (other than arizona)
PE: sat 93% on RA; o/w unremarkable
PFT's: FEV1 1.60 (77%)
FVC 2.04 (74%)
FEV1/FVC 79% (105%)
TLC 4.51 (92%
RV 49 (109%)
DLCO 10.28 (45%)
Radiographs:
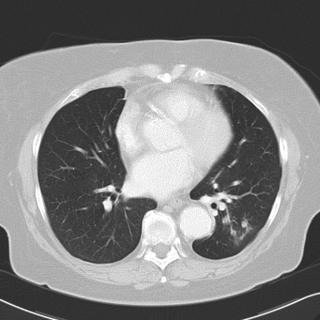
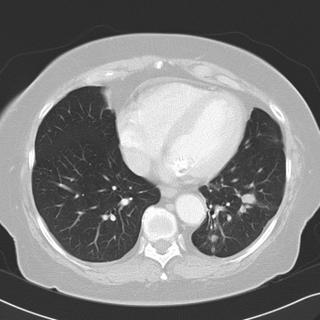

Chest CT's in the past (i.e. before her trip to Arizona) do not show any pulmonary abnormalities. She has gotten serial Chest CT's to follow her aneurysm.
What would you do next?
4 comments - CLICK HERE to read & add your own!:
I think it's fairly rare to get respiratory failure from coccidio, especially if you're not immunocompromized. The nodules on the CT look pretty typical for the disease though. Maybe she had another reason for the respiratory failure and she ALSO had been exposed to coccidio from being in arizona and hence the positive BAL finding.
In any case, it seems now she is doing fairly well with just some mild spiro abnormalities and a good saturation on room air; I would justy follow on the sidelines and put her in a pulm rehab program.
I think that acute respiratory failure can occur with coccidio...however, I would have expected her to recover in 8 months. Further, I don't think that her room air pulse ox of 93% is entirely normal. Her PFT's are not diagnositic of restriction, but the decreased FVC and increased FEV1/FVC does jump out, even with the normal TLC. The DLCO is markedly low.
The CT scan shows some nodules in the LLL, and there looks like a mild left pleural effusion or possibly pleural thickening.
The CT scan findings could be the sequalae of a prior infection. Given here recent cardiac intervention, her continued dyspnea is unlikely to be cardiac in nature, but you havn't given us an indication of her post-intervention cardiac function.
I'd consider a CPET here, and am concerned about a pulmonary vascular problem given the very low DlCO. Depending on the CPET results, I'd consider a biopsy of the larger left peripheral nodule, a HRCT, possibly a V/Q scan, and an echo.
Respiratory failure can occur in healthy people. Extensive pneumonia with failure occurs in cocci either in immunocompromised hosts or in immunocompetent hosts who get a large inhaled inoculum from heavily contaminated soil.
There is an entity of "chronic pneumonia" in cocci which, I think, is quite rare (<5%) when there is fatigue (and sometimes chronic respiratory symptoms) for weeks and months beyond the original presentation. However, I don't remmember if 8 months would be within that window.
Is she still on an antifungal? Unlike histo and other endemic fungi, treatment often needs to be longer with cocci, especially in someone who was this sick and she may have been undertreated and those nodules represent chronic disease.
Having said that, JJ and JH raise the excellent point that she may have something else going on...
Sorry it took me so long to finish this case. WBH internet access has been very slow b/c of computer updates.
I also agree with everyone that something else may be making her dyspneic.
I neglected to mention that she had a DVT diagnosed when she was in AZ during her hospitalization.
When I saw her in f/u, she was on ASA and plavix (for her stent and CAD) and warfarin for her DVT. PE is treated.
The most recent CT scan had 3 mm cuts, and there was not even a hint of ILD. So, my suspicion of occult ILD is small.
The only thing that I could do to w/u an isolated DLCO problem would be to get a sleep study to r/o OSA and associated pulm HTN. I set this up.
As far as the fluconazole, she was on homeopathic doses when she came to f/u. Carlos' entry regarding the duration of treatment of coccidiomycosis is the real teaching point which I did not know... often you have to treat for 1-2 years with fluconazole 200 q Day for this disease. Carol Kauffman at U of M has several review articles discussing this exact point. However, as she was doing better after her PTCA, I decided to stop the medicine. She was undertreated for the last 4 months anyway.
I will repeat the scans (or actually, just watch her scans for her aneurysm) and react to the nodules if they change or more develop.
Does anyone have any other thoughts that may be helpful for me?
Post a Commenttest post a comment