34 y/o AA woman with pancytopenia 10 years ago. Asymptomatic, lost to f/u because of insurance. Refused BM biopsy. 5 years ago gradual onset of dyspnea. May of this year presented with SOB and admitted. (Pulmonary consult called at that time). On exam she had some JVD, clear lungs, loud O2, hepatosplenomegaly, ascites and 2+ pitting edema. Echo showed PAP of 48 with dilated RV and an LV with an EF of 65%. Labs: WBS 2.2 with 82% N, Hgb 9, plts 104. ACE was 207.
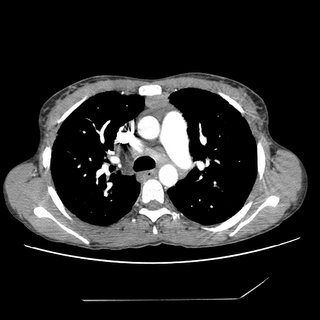
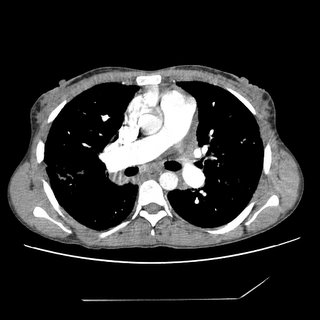
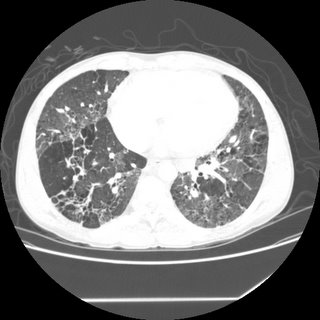
CXR and CT:



Bronch BAL not sent, therefore cell count and micro of the fluid unknown. A TBBX showed of the RNL showed a single poorly formed granuloma. The micro on the biopsy *was* sent and was negative. Endobronchial biopsy showed active chronic inflammation.
Urinary histo Ag never sent. Serum Ab's against fungus also not sent.
Questions:
1. Would you consider the above info sufficient stop at the diagnosis of sarcoid?
2. Would you be satisfied with no infectious cause based on negative Tbbx micro, but BAL not sent?
3. Do you feel that a cell count with CD4 and CD8 would have been helpful to you?
4. (corollary to 1): Is there anything else on your differential list besides sarcoid? The person presenting this case to me has no other diagnoses on his list.
5. Does the history of 10 years of pancytopenia rule out histoplasmosis or other fungus?
4 comments - CLICK HERE to read & add your own!:
Cool case.
She needs a bone marrow anyway to w/u her pancytopenia (I would not assume that is sarcoid related), and this will likely show granulomas. Also, culture of the BMBx is pretty sensitive and specific for fungal disease in a setting of pancytopenia. It would be hard to believe that she had active histo for 10 years without getting worse, however. You could send serologic fungal studies if you think it may be helpful. The BMBx would be all that I would need.
If she is afebrile, I would not be inclined to BAL her again. If it was positive for S. Aureus, would you treat? I would not. She should not have gradual dyspnea with a pulmonary infection.
A CD4/CD8 would not be helpful.
Other things in the DDx: CVD with associated ILD. I cannot think of anything else. Maybe CEOB has a worm/parasite in mind.
1. I agree with ML, I would not be satisfied with sarcoid as the only Dx.
2. I don't think that "incomplete" BAL sampling rules out infection.
3. If the cell count had a predominance of CD8s with that loose granuloma, HP could account for some of the parenchymal changes and sarcoid would be less likely the cause.
4. I think there are two questions on the DDx: what caused the pancytopenia in the first place? and are the infiltrates caused by the same entity? At age 24 (onset of pancytopenia) there are several possibilities: drug-exposure such as "huffing" toluene/benzene can lead to this presentation but she would not have lived this long. Same for AML. Viral etiologies don't seem to fit well either: Parvo B19 should be self-limited and HIV and HEPC would have progressed after 10 years... Young adults with aplastic anemia due to one of the agents above can progress to MDS and that might explain her protracted course. PNH could also explain this presentation though they tend to have renal and thromboembolic Dz too. Maybe the mosaic appearance with the Pulm HTN are due to chronic VTE due to PNH (check a Ham test).
5. "Chronic" histo for 10 years with stable bone marrow disease seems an unusual presentation...
For Mike's sake, visceral Leishmaniasis will cause this picture of pancytopenia though I doubt she has been bitten by sandflies in the Middle East or South America...
1. No, that is not enough for sarcoid. The differentials listed (endemic fungi, HP, Collagen-vascular associated ILD) have not been excluded. Lymphoma is unlikely, although we don't really know how long the mediastial LAD has been there.
2. No, the BAL does not exclude infection, although as Mike and Carlos noted, I doubt active infection in the lung now, if present, would be related to the pancytopenia. I'll also note that while she is not absolutely neutropenic, we don't know if her white cells "work" normally.
Has HIV been checked?
3. As Carlos noted, a low CD4/CD8 (less than 2) would support HP, while a high ratio can be seen with sarcoid. But, I would not pin any diagnoses on this.
4. See #1 above.
5. The pancytopenia sounds like it's been stable over the years, but the lung findings have progressed. Not sure they are directly related. I think a bone marrow biopsy AND a surgical lung biopsy should be done.
I'd love to hear from some of the non-regulars out there!!!
Post a Commenttest post a comment