I don't keep up with the non-pulmonary allergy literature as I should. I often see atopic patients with or without true asthma who have allergy testing and then are started on allergy shots for desensitization. I have just seen someone who has been getting those three times a week for the past 6 years.
How often do you use allergy testing or shots in your practice? Any good literature on that in pulmonary practice?
Thursday, April 27, 2006
PEEP
Today's NEJM's cover article is by Gattinoni et al and they have looked at the ammount of "recruitable" lung in the setting of ARDS. This is after the results from the ALVEOLI study on High-Low PEEP.
How do you use PEEP in your ARDS patients? Have you been trying to "recruit" more lung with higher PEEP? Since the patients on the High PEEP did not have worse outcomes are you more comfortable with higher PEEP when oxygenation is a problem?
How do you use PEEP in your ARDS patients? Have you been trying to "recruit" more lung with higher PEEP? Since the patients on the High PEEP did not have worse outcomes are you more comfortable with higher PEEP when oxygenation is a problem?
Wednesday, April 26, 2006
Physiology question
I am hoping to stimulate some discussion involving a simple question with complex pulmonary physiology.
2 questions involving a patient with COPD who is a known CO2 retainer (pCO2 around 50-60 with a preserved pH) at baseline:
1. Why can putting them on high flow oxygen (i.e. when they present to a Emergency with increased dyspnea) worsen their CO2 retention?
2. How do you know how much oxygen to give these individuals if they are truly hypoxemic?
2 questions involving a patient with COPD who is a known CO2 retainer (pCO2 around 50-60 with a preserved pH) at baseline:
1. Why can putting them on high flow oxygen (i.e. when they present to a Emergency with increased dyspnea) worsen their CO2 retention?
2. How do you know how much oxygen to give these individuals if they are truly hypoxemic?
Follow up to Nodule and Mass
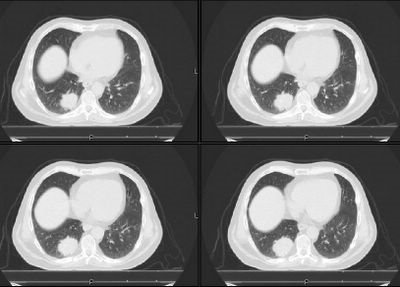
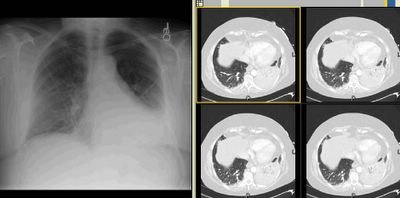
I had posted this but didn't get much feedback. This is the fairly healthy 40 y/o woman with some chronic back pain but no pulmonary or cardiac disease referred to us for a "new" pulmonary mass. She has never smoked and has had no pulmonary symptoms. She had been told about 10-15 years ago that she had a calcified R lung nodule and that has just been followed along. However she had had recent imaging for her back and they found that mass in the azygoesophageal recess.
Jennings astutely pointed out that the posterior mass looked very heterogeneous and almost cystic. The films were outside films so we decided to try a bronch and a repeat CT. Our radiologists felt comfortable that the peripheral lesion looks like a hamartoma and agreed the mass appeared cystic like a bronchogenic cyst. The bronch (we tried some FNA passes. Was fairly unremarkable and essentially non-diagnostic.
Would you have done something else? Would you consider a PET? If negative we might not repeat imaging studies as frequently... Or would you even bother with scheduled CTs if she remains asymptomatic?
Jennings astutely pointed out that the posterior mass looked very heterogeneous and almost cystic. The films were outside films so we decided to try a bronch and a repeat CT. Our radiologists felt comfortable that the peripheral lesion looks like a hamartoma and agreed the mass appeared cystic like a bronchogenic cyst. The bronch (we tried some FNA passes. Was fairly unremarkable and essentially non-diagnostic.
Would you have done something else? Would you consider a PET? If negative we might not repeat imaging studies as frequently... Or would you even bother with scheduled CTs if she remains asymptomatic?
Monday, April 24, 2006
Pulmonary nodule
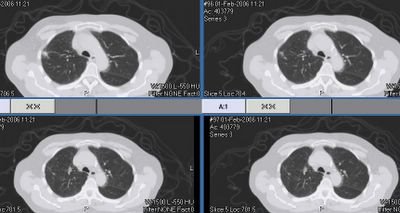
This 44 y/o man is one of our former nurses. He had gone to Florida on vacation and came back with an infectious diarrhea. The ER did a CT scan of the abdomen and they found a pulmonary nodule on the lower lung cuts (see below).
He has no respiratory symptoms whatsoever. He quit smoking in 1988 and had about a 10 pack-year total.
What do you think of the nodule (it is 11x12 mm) and what would you do next?
He has no respiratory symptoms whatsoever. He quit smoking in 1988 and had about a 10 pack-year total.
What do you think of the nodule (it is 11x12 mm) and what would you do next?
Abnormal CT and hypoxia.
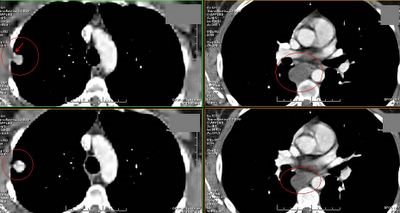
38 year old white female with PMH of interstial cystitis presented to ER by EMS after she was found to have a seizure at home witnessed by her mother. That was her second seizure and her initial one was 1 month ago when she went to an outside local hospital. Her work up at that time included head CT which was negative except for sinus disease. She was advised to follow up with her PCP at that time.
In the emergency room, she was afebrile but post-ictal. She was also hypoxic. She was put on oxygen and admitted.
PmHx only significant for the interestitial cystitis. Had some ankle edema 6 years ago treated with low salt diet; thought secondary to her job standing all day (dishwasher).
Medications: none.
CT scan: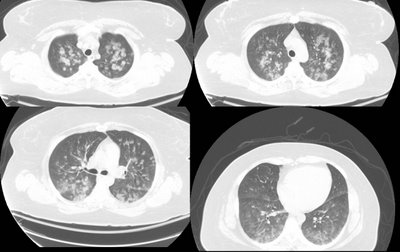
RF and sed rate low or normal.
What are your thoughts and what would you do?
In the emergency room, she was afebrile but post-ictal. She was also hypoxic. She was put on oxygen and admitted.
PmHx only significant for the interestitial cystitis. Had some ankle edema 6 years ago treated with low salt diet; thought secondary to her job standing all day (dishwasher).
Medications: none.
CT scan:
RF and sed rate low or normal.
What are your thoughts and what would you do?
Thursday, April 20, 2006
Sarcoid: treat now or diagnose first?
Dr Curry would like to know:
In a 42 year old African-American woman with symmetric bilateral hilar adenopathy symptomatic (dyspnea on exertion), and an eye exam "consistent with sarcoid", would you treat (steroids) based on this or would you first proceed to TBBx for confirmation of the diagnosis? Of note, her spiro is normal.
In a 42 year old African-American woman with symmetric bilateral hilar adenopathy symptomatic (dyspnea on exertion), and an eye exam "consistent with sarcoid", would you treat (steroids) based on this or would you first proceed to TBBx for confirmation of the diagnosis? Of note, her spiro is normal.
Steroids and ARDS
The ARDSNet just published the results of the Corticosteroid trial on the NEJM.
There was no mortality benefit and actually there was increased mortality in those started "late" on steroids.
Had you been using steroids on ARDS and/or is this new study going to change your practice?
There was no mortality benefit and actually there was increased mortality in those started "late" on steroids.
Had you been using steroids on ARDS and/or is this new study going to change your practice?
Wednesday, April 19, 2006
Categories
We now have categories - the goal will be to categorize each case based on topic (i.e. interstitial lung disease, pulmonary nodules, etc.). We use a program called Linkr to do this. The only problem is that comments are not displayed with the cases. However, you can get around this bug by clicking the date/time stamp at the bottom of the post. This "permalink" will then display the case with all comments attached.
If you have suggestions for categories please leave a comment here.
If you have suggestions for categories please leave a comment here.
Tuesday, April 18, 2006
Nodule and mass
This images are from an outside radiology service so the quality suffered a bit when I copied it...
This is a fairly healthy 40 y/o woman with some chronic back pain but no pulmonary or cardiac disease referred to us for a "new" pulmonary mass. She has never smoked and has had no pulmonary symptoms.
She had been told about 10-15 years ago that she had a calcified R lung nodule (left pics) and that has just been followed along. However she has had recent imaging for her back and they found that mass in the azygoesophageal recess (right pics).
Would you be concerned? Do you think the two lesions are related and what is your differential?
DVT/PE
This was brought up this week:
"Does anyone know the reference for a study that showed in patients who were asymptomatic from a cardiopulmonary perspective but had a positive LE doppler for a DVT the incidence of documented PE on a PA-gram?
I know there is a study showing this, but I cannot find the reference."
"Does anyone know the reference for a study that showed in patients who were asymptomatic from a cardiopulmonary perspective but had a positive LE doppler for a DVT the incidence of documented PE on a PA-gram?
I know there is a study showing this, but I cannot find the reference."
Monday, April 17, 2006
Percutaneous trachs
Have you had much experience or come across data on percutaneous (vs open surgical) trachs in you persistent respiratory failure ICU patients?
Symmetric bilateral hilar adenopathy
47 year old African-American man who was asymptomatic at the time of this chest xray:

His PFT's were normal. LFT's were slightly elevated (Alk phos 192, GGT 152) with a normal ultrasound and no abdominal complaints. A presumptive diagnosis of sarcoidosis was made and the patient was simply followed. 5 months later he c/o subjective fever and night sweats. No respiratory symptoms. A chest xray was actually improved:

What would you do? Are you still satisfied with the diagnosis of sarcoid? (I am aware of a study that found that in almost all cases with symmetric adenopathy, the dx is sarcoid.) WOuld you want to definitely dx it or rule out other causes?
If you are satisfied with the dx, how would you handle the constitutional symptoms? Assuming f/u PFT's are not in decline, would you treat these B symptoms with immunosuppressive therapy?

His PFT's were normal. LFT's were slightly elevated (Alk phos 192, GGT 152) with a normal ultrasound and no abdominal complaints. A presumptive diagnosis of sarcoidosis was made and the patient was simply followed. 5 months later he c/o subjective fever and night sweats. No respiratory symptoms. A chest xray was actually improved:

What would you do? Are you still satisfied with the diagnosis of sarcoid? (I am aware of a study that found that in almost all cases with symmetric adenopathy, the dx is sarcoid.) WOuld you want to definitely dx it or rule out other causes?
If you are satisfied with the dx, how would you handle the constitutional symptoms? Assuming f/u PFT's are not in decline, would you treat these B symptoms with immunosuppressive therapy?
Saturday, April 15, 2006
Follow-up to What is your algorithm?

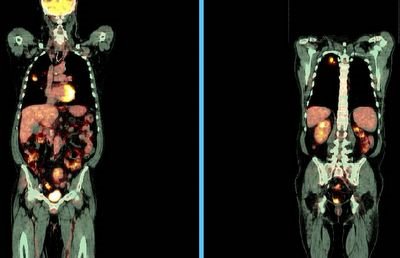
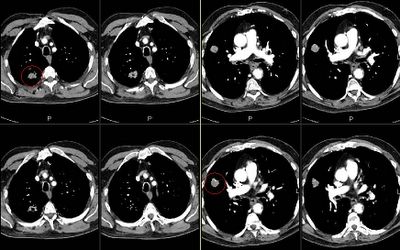
This is the 64 y/o man with significant TOB Hx and a lung mass.
I had the same thoughts as Jeff H.
His FEV1 incresed to >2L (>60%) on Spiriva. A bronch revealed no endobronchial lesions but was otherwise non-diagnostic. The PET lit up up (brightly, see above) only on the mass and nowhere else.
What would you do next?
Thursday, April 13, 2006
What is your algorithm?
This is a 64 y/o man with a 100-pack-year TOB Hx referred to us for a lung mass found on a CxR for cough. His CT is posted above. The mass is the only abnormality. There is no associated adenopathy.
His FEV1 on no bronchodilators is 1.96L (55%) and he has no other medical problems.
How would you evaluate him? PET, cut, scope?
Wednesday, April 12, 2006
Categories
Today is the roll-out of categories. I am working on sorting all previous posts into categories (ILD, COPD, etc. see column on right).
A post can have more than 1 category. I have only done a few so far. Also, please fill out the survey (see link to right) because we would like to identify barriers to posting comments and cases. You can also reply to this post as well....
A post can have more than 1 category. I have only done a few so far. Also, please fill out the survey (see link to right) because we would like to identify barriers to posting comments and cases. You can also reply to this post as well....
Follow-up to abnormal CT scan
This is the post below with the abnormal CT scan and PET with positives nodes.
She had a non-diagnostic bronch and a non-diagnostic supraclavicular node Bx. All Cxs have been negative.
She underwent a mediastinoscopy and all nodes sampled had necrotizing non-caseating granulomata with negative AFB and GMS stains.
What would you do next?
She had a non-diagnostic bronch and a non-diagnostic supraclavicular node Bx. All Cxs have been negative.
She underwent a mediastinoscopy and all nodes sampled had necrotizing non-caseating granulomata with negative AFB and GMS stains.
What would you do next?
Tuesday, April 11, 2006
Pulmonary function
How would you define these pfts? The ratio is 72 (96% predicted). FEV1 63% pred and FVC 65%.
The TLC is 84% predicted and the DLCO is 44%.
The TLC is 84% predicted and the DLCO is 44%.
collapsed RML
Check out Jeff's post below.
I hate to answer a question with another question, Jeff but I have had this similar case. This is a 65 y/o woman, no significant TOB Hx with recurrent partial LLL collapse. She has had LLL CAP 3 times (see above) and though the pneumonias clinically all resolve (they have been over ~ 5years) she always has a residual partial LLL collapse. She was bronch'ed in 2001, 2002 and I have re-bronch'ed her in 2005. Her airway though a little narow with some dynamic collapse looks normal and biopsies and Cxs were also all negative.
Other than encouraging pulmonary clearance, chest P&PD, etc. would you do anything else?
I hate to answer a question with another question, Jeff but I have had this similar case. This is a 65 y/o woman, no significant TOB Hx with recurrent partial LLL collapse. She has had LLL CAP 3 times (see above) and though the pneumonias clinically all resolve (they have been over ~ 5years) she always has a residual partial LLL collapse. She was bronch'ed in 2001, 2002 and I have re-bronch'ed her in 2005. Her airway though a little narow with some dynamic collapse looks normal and biopsies and Cxs were also all negative.
Other than encouraging pulmonary clearance, chest P&PD, etc. would you do anything else?
collapsed RML
A 62 year old smoker presents with RML collapse. A bronchoscopy is negative to endobronchial lesion. Cytology and micro are negative. She is treated for pneumonia and released. A few months later the CXR is essentially normalized excepts for some left over streaking.
Would you do anything else or not?
Would you do anything else or not?
Monday, April 10, 2006
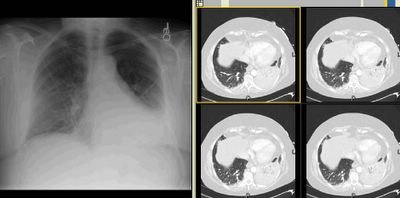
Abnormal CT scan
We were asked to see this delightful 67 y/o woman with no respiratory symptoms for an abnormal CT scan of her chest. She has had some back pain and a nodule was found on a CxR. The CT scan above was obtained and she was referred to us. She quit smoking in 1992.
She has good lung function with normal FVC and FEV1~ 70%.
She was set up for a PET scan and the images are seen below:
I don't know if the writing projects well but the RUL lesion is positive and she has positive paratracheal and R hilar nodes. There was also a positive 4-mm R supraclavicular node that did not project well.
What would you do next?
Friday, April 07, 2006
Radiology Friday. 20 year old female
Wednesday, April 05, 2006
Unexpected findings
A 59 year old man was referred for an unexpected finding in the RUL discovered during an operative airway exam prior to resection of a large left lung mass. The lung mass turned out to be a solitary fibrous tumor. We were asked to evaluate the unexpected lesion in the right upper lobe. At bronchoscopy, I saw a lesion at the very proximal anterior segment of the RUL.

This was adherent and non-mobile. The patient is otherwise healthy, and his immune-system is intact.
Thoughts?

This was adherent and non-mobile. The patient is otherwise healthy, and his immune-system is intact.
Thoughts?
PTx

This is just a quick show-and-tell (though feel free to comment).
This is a 73 y/o heavy smoker transferred from an outside hospital with a PTx. He had a CT placed there but had a large persistent leak and was transferred for further evaluation. His outside CT showed lower lobe predominant bullous emphysema with a large RLL bulla. (unfortunately those were outside films and I couldn't post them).
He was started on aggressive bronchodilator therapy and stabilized. His spiro revealed a severe obstructive ventilatory defect. He underwent a bullectomy and the CT surgeon got these great pictures:
He is doing very well. His BPF has closed with the lobectomy and his dyspnea is much improved.
Tuesday, April 04, 2006
Synchronous lesions or intralobar M1?
This is a 65 y/o man with a long Hx of TOB use with moderate COPD. We were consulted after a CT-guided Bx of one of his RUL masses revealed a NSCLCa (see masses above, both are in the RUL). A PET scan (see below) revealed increased uptake by both masses but nowhere else.
His PFTs would easily allow a lobectomy.
How would you approach him? Does it matter whether we call this intralobar M1 or two separate synchronous lesions?
Final diagnosis and results below in the discussion.
Monday, April 03, 2006
Like father like son...
Subscribe to:
Posts (Atom)