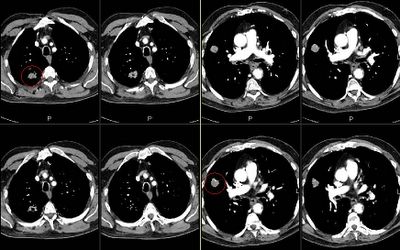
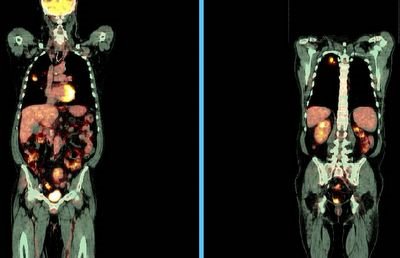
This is a 65 y/o man with a long Hx of TOB use with moderate COPD. We were consulted after a CT-guided Bx of one of his RUL masses revealed a NSCLCa (see masses above, both are in the RUL). A PET scan (see below) revealed increased uptake by both masses but nowhere else.
His PFTs would easily allow a lobectomy.
How would you approach him? Does it matter whether we call this intralobar M1 or two separate synchronous lesions?
Final diagnosis and results below in the discussion.
5 comments - CLICK HERE to read & add your own!:
In a case like this, I would be inclined to give him the benefit of the doubt (i.e. he has 2 stage IA lesions).
So, I would hope your surgeons are willing to give him a shot with a lobectomy.
I think an equally interesting question is whether to give this man chemotherapy in the post-op period. It would definitely be offered if he had IB or higher staged disease, so would 2 nodules change the course?
That's a tough call. I agree with Mike. I think lobectomy should be pursued because surgery is the only curative option and there is still the possibility that we have two stage IA lesions. He has good lung function and would not be a high surgical risk.
On the other hand, if they are M1, treatment is only palliative anyway, so I would err to the option that has cure as a possible outcome.
We would also err on the side of treatment, unless the patient has extensive co-morbidities. In a patient with good functional status, good PFT's, and no evidence of extrathoracic disease, we would probably proceed with lobectomy.
I think Mike's question of adjuvant chemotherapy for synchronous 1A primaries is a good one. With no evidence whatsoever to back this up, if I were the patient I would want the adjuvant chemo!
Is that the royal we?
Well, great input. His PET as noted in the post showed no other distant Dz. Ct of head was normal with no neuro symptoms.
We (the royal we) also favored resection. He did very well and his final path showed: multiple nodes (including intralobar, bronchial, hilar and mediastinal all negative (some from the med, some post-op). The more apical mass was a 2.5 cm mod-to-poorly differentiated squamous cell Ca >5cm from the nearest margin and the lower lesion was a 2.3 cm mod-to-well differentiated locally invasive adenoCa > 1cm from the nearest margin.
I think adjuvant Tx seems to be the consensus and that was also our suggestion.
Post a Commenttest post a comment