Past medical history is significant for coronary artery disease, status post MI 11/2005, hypertension, diabetes, breast cancer 7/2004(5-FU,cytox, Mtx) s/p xrt, and chronic renal insufficiency.
SH; ex smoker. Occupation: Did military work.
meds: CAD meds and some inhalers etc.
Over the last few months her dyspnea worseneed and she is now on 6 L of oxygen 24/7.
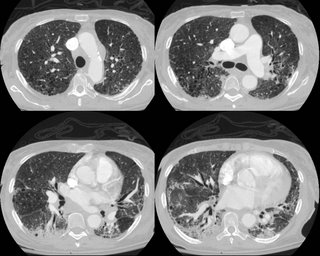
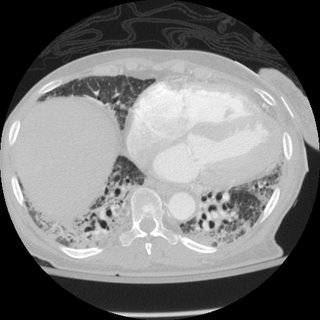
Here is a CT from last month:
What do ye all think is going on?
6 comments - CLICK HERE to read & add your own!:
CT is ugly, but it is not a classic appearance for UIP.
Can you offer us a little more history:
1. Drugs that cause fibrotic lung disease (nitrofurantoin, amiodarone,
2. What was her military job (i.e. beryllium exposure, work on a ship with asbestos exposure, etc.)
The differential diagnosis is large including ILD (either primary/idiopathic or secondary), chemotherapy toxicity, HP, infectious (although lack of systemic symptoms and 6 month history makes this less likely), chronic aspiration.
There is an incidence of BOOP after XRT from breast cancer, so I suppose this should be in the DDx.
I would bronch, BAL and TBBx.
If /when this is negative, I would get a Surg lung biopsy.
There are thin walled cystic changes in the upper cuts. They have fairly low attenuation and thin walls and in the first cut could be emphysematous changes from her smoking. As the cuts progress they seem to blend in with the inflammatory/ILD changes. I agree with Mike that it does not look classic for UIP and you need tissue. I also like Mike's suggestion of chronic aspiration. Any interesting family Hx?
I will expand the history slightly; the XRT for her breast cancer stopped about 5 months before the onset of her dyspnea (and radiogrpahic changes)....
I think Mike mentioned post xRt changes on his first comment. She may have some underlying COPD and now has post-radiation pneumonitis too...
Yes. I'm not sure if you would call it BOOP or COP or radiation oneumonitis or whether it even matters. I elected to treat her with steroids and we'll see how she does.
A bronchoscopy a month into her symptoms showed on TBBx focal acute bronchial inflammation. The WBC's in the BAL were 62% macrophages and 32% neutrophils.
I doubt that this is XRT pneumonitis.
This entity rarely occurs outside the radiation port, and you have radiographic evidence of disease in both lung fields.
BOOP has only been shown s/p XRT for breast cancer. It can be seen outside the radiation ports
Criteria for diagnosing COP syndrome
1. XRT for carcinoma (breast) within 12 months
2. Respiratory symptoms lasting at least 2 weeks
3. Radiographic infiltrates outside the lung ports
4. No obvious alternative diagnosis
In the cases of BOOP related to XRT, a tissue diagnosis does not need to be confirmed.
How did she do clinically after steroids?
Post a Commenttest post a comment