
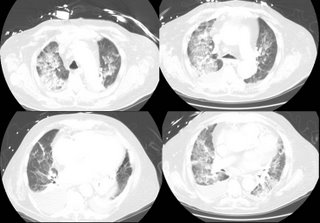
He then developed SIRS (WBC, fever, tachy) but no infectious source ID'd. He was intubated. A CT is here:
 .
.A month later he is still intubated with the following CXR:

What is your differential diagnosis? What tests/procedures/other data would you like to know?
2 comments - CLICK HERE to read & add your own!:
Well, this is not much to go on from a historical/diagnostic perspective, so the diagnosis is as broad as your left... well, let's just say it is broad.
Other info that would be valuable:
1. Any cultures
2. A pre and post surgery echo
3. PA catheter/CVP readings (if available)
4. Any bronchoscopy results
5. Results of thoracentesis
6. Urinalysis results
7. Has he had a splenectomy?
His initial CXR showes a bilateral interstitial pattern with a left pleural effusion. His chest CT while in respiratory failure shows bilateral alveolar disease process with right > left pleural effusion.
This could represent
1. CHF
2. Non-cardiogenic pulmonary edema
(ALI/ARDS)
3. An infectious process NOS
--Remember he is immunosuppressed given his prednisone dose for ITP and probable stress dose steroids around the surgery
--More concerning for encapsulated organisms if he has had a splenectomy
4. A vasculitis/inflammatory process in the lung (SLE, ANCA(+) vasculitis, Goodpastures, etc)
I would get the tests that would help identify the processes above. If it is not done, bronch with BAL (looking specificially for eosinophils and culture results). If you have access to a CVP, it would be helpful; also EDM data (if performed at HFH) might give some info.
Thanks. Nice thorough off-the cuff ddx. His diffuse b/l airspace disease coincided with as rising white count and some other criteria that fit SIRS, so I was thinking sepsis-associated ARDS. No micro source so I BAL'd him - absolute neutrophil count was 3000. CMV shell was positive. I emprically treated with gancyclovir (would anyone confirm CMV by biopsy? I chose not to given his severe illness I didn't want to give him a chest tube too).
After a week on gancyclovir, the serum CMV antigen(PCR)came back positive.
My final diagnosis is ventilator-dependent respiratory failure secondary to CMV pneumontis, which was due to his chronic steroid use from the ITP. BTW, no, he has not had a splenectomy - his outside hematologist has been treating with 40 of prednisone for years.)
Post a Commenttest post a comment