Exam: A pleasant woman in no acute distress. WT of 197, BP 185/83, P is 65, R 18, O2 sat is 97% on room air. Trachea midline. No lymphadenopathy and no supraclavicular adenopathy. No thyromegaly. Lungs: Clear to auscultation. No wheezing, rales, or rhonchi. No dullness to percussion. No egophony, symmetric chest wall on inspiration. Heart: Regular rate. S1, S2. Abdomen: Positive bowel sounds. No masses. No liver edge felt. No clubbing, cyanosis, or edema.
Data:
PFT's: FEV1/FVC 81, FEV1 76% predicted, FVC 73% predicted.
CBC with hemoglobin of 10.3, MCV of 94.6. Plts normal. Lytes-7 normal. ANA and rheumatoid factor negative
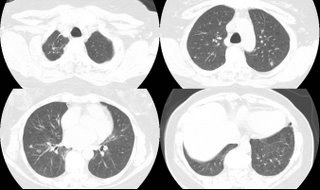
These nodules are all non-calcified. The largest is 8 mm. There is interval growth of left lower lobe nodule and right apical nodule compared to a CT 6 months prior. The subcarinal soft tissue is "prominent" but ambiguous whether it's enlarged.
On abd CT, the spleen, pancreas, kidney, gallbladder and adrenals are unremarkable.
2 calcified hepatic granulomas are seen.
Any thoughts on workup or management?
.
4 comments - CLICK HERE to read & add your own!:
Well, with the calcified granuloma in the liver, can't this be fungal? Also, she's a non smoker and the abdominal CT didn't show any cancer in terms of worrying about metastitic disease.
If it was metastasis (i.e.from the breast) and they were present 6 months ago, one would think she would be sicker. Also, post mentioned no adenopathy although I agree that fact alone does not necessarily rule out metastatic cancer.
My suspicion for mitotic process is not high either. Starting with routine cancer screening (i.e. mammogram, pap smear, colonscopy) may be an option if not done recently.
In view of the finding as described the chances of metastasis or primary lung cancer are high. It possible and one can go for CT guided FNAC coorectoly can sove the problem to some extent. In the mainwhile the work to find the primary somewhere else is worth doing as mentioned by rednec pulmonary.
Post a Commenttest post a comment