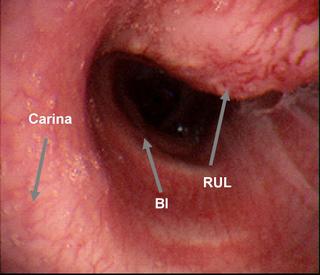
So, I met the patient a few days later when he came down for a bronchoscopy. No sputums had been obtained, and no drugs had been started. Personally, I felt strongly that the patient should have been started on 4 drugs the minute he hit the door. Here's what I saw...
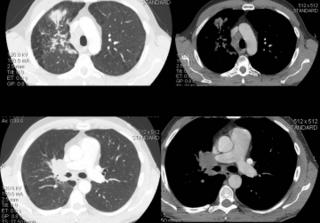
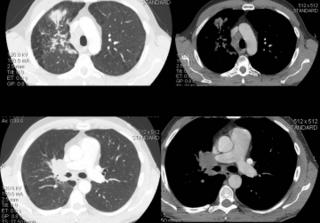
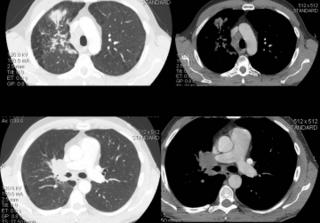
A CT was done:
Answer in the comment section below.
8 comments - CLICK HERE to read & add your own!:
No comments???
Yeah, when are you going to check your own PPD?
That endobronchial lesion seems to be the hilar mass/adenopathy almost trying to erode through the bronchial wall.
Common things being common, he is a smoker and that could be a bronchogenic Ca in which case the spinal process may or may not be related.
The granulomatous infections we have mentioned could look like that as the necrotic lymphnode erodes through the mucosa.
Are you PPD +?
I suppose that I fail to see the urgency in the bronchoscopy. If this is cancer, the patient has a T4 lesion (A minimum 2 synchronous lesions in the same lobe). That makes him unresectable. Or, I suppose it could be a T2N1 lesion with obstructive pneumonia (IIB) that would be resectable.
Anyway, it still does not change the fact that 3 days probably will not make any difference in this lesion metastasizing. Oh, and if it were lung cancer, it may have already done that. As such, it would be better to go after the met in the spine (provides diagosis and stage).
So, plenty of time to get 3 AFB's. And start 4 drugs.
If it is sarcoid, fungus or one of those weird parasites that CEOB sees, it can wait.
The only thing that NEEDED to be diagosed first was TB.
That lesion appears to be very vascular. Did you sample it?
Nana-na-na-nana.
For the record, I suggested a fungus this time, not a parasite...
As it turns out, the lesion shown was completely obstructing the RUL bronchus. I did sample it, with brushings (for both micro and cytology), washings, and with endobronchial biopsies (3). It did bleed some, but not very badly.
Although I agree completely with Lazar, and did not see the need for bronch that quickly, this was not TB. Remeber, the CT scan was done after the bronch...as it turns out, this was all non-small cell carcinoma (including the lumbar-spine lesions).
I posted this one now because it illustrates a crucial point. Carlos just presented a case that we all were positive was a carcinoma; it was TB. In this case, I, like all of you, thought this as slam-dunk a diagnosis of TB as I would ever see. Of course, it was carcinoma.
Bottom line: we need to make sure we evaluate these patients completely in all cases, as our first impressions are frequently wrong...
Post a Commenttest post a comment