About 2 days into her hospital course, she was undergoing a regular hemodialysis run, when she had a cardiac arrest. She was in PEA, and was resussitated with epinephrine x 1 and IVF x 500 cc. She was intubated and brought to the MICU.
Upon arrival, she was noted to have an episode of massive hemoptysis (~200 cc). A post intubation film showed the tube in a good position (see film). The episode was limited without intervention. A second episode occurred (~300 more cc) just prior to the bronchoscopic examination.
PAST MEDICAL HISTORY: Ascending / Descending aortic aneurysm status post repair (unclear what was used as the old records had not been faxed prior to her decompensations), endstage renal disease, for which she is on hemodialysis, recent cerebrovascular accident with resulting encephalopathy, right groin ulcer, hypertension, history of cocaine use, hepatitis-A, hepatitis-B, hepatitis-C, enterococcal bacteremia and recent jejunostomy dislodgement.
PE:
Hypotensive on Norepinephrine (20 mcg) with SBP ~90; sinus tachycardia 136; Saturations unobtainable b/c of cold extremities (ABG during code with PO2 of 200).
Radiographs:
 Admission
Admission  After intubation
After intubation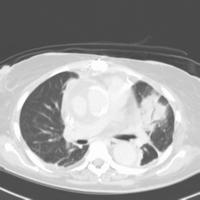 CT 2 days prior to intubation
CT 2 days prior to intubationDifferential Diagnosis?
Inteventional plan?
4 comments - CLICK HERE to read & add your own!:
The post xray looks like the mediastinum on the right is wider. On the CT is seems that there is quite a bit that cannot be ascribed to tissue, and (although this may be from the resolution), the complete ascending aorta cannot be seen - maybe there is bleeding into mediastinum? With his prior history of aortic grafts, perhaps there aneurysm. A fistula would then have to be postulated to account for the hemoptysis. What did the bronch show, especiaially in the trachea and main stems? Sounds like he needs a TEE and then surgical intervention.
Actually that infiltrate/lesion in the left upper lobe may be the source of the bleeding if my above idea is completely wrong.
JJ raised an excellent point about aorto-bronchial fistula, with graft eroding onto the bronchial wall. Those have a very dramatic presentation. The are of infiltrate seems very focal and not diffuse as I would expect from crack/cocaine lung if he were using again.
The infiltrate may also be the source of the mucosa erosion and a "simple" pneumonia may have led to the hemoptysis in a vasculopath.
The hepatitides add an element of interest though I don't think I saw a reference to abnormal coags. Mixed cryoglobulinemia associated with Hep C and PAN with Hep B may cause vasculitides though this does not appear to fit too well with the case.
I agree that a TEE would be a great start and certainly safer than to take him down for an MRA.
Do you have any f/up for us?
I bronched her and she had blood everywhere in her pulmonary tree. It was clearly coming from the LUL proper and was "welling up" fairly quick.
She rapidly deteriorated over the next 1 hour with hypotension and hypoxemia. She coded on the way to interventional radiology to try to stop the bleed.
An autopsy showed essentially nothing grossly. I am still awaiting the histo. Hopefully, I will know more in the next 1-2 days.
Both JJ and CEOB recommended at TEE; what would that tell you?
Post a Commenttest post a comment