Her cough was dry so we could not get any sputum samples. I was also concerned about lymphoma. However, since her lung was not trapped, I did a bronchoscopy first rather than a VATS. Especially because that more anterior infiltrate seems like a real infiltrate and not just compressive atelectasis.
Her TBBx showed non-specific inflammation and no malignancy. Cytology was not helpful. Smears were negative for AFB and fungi but + for GPCs and Cxs came back + for MRSA (kind of a "community-acquired" MRSA: RR to beta-lactams but SS to everything else).
She felt much better and wanted to go home.
Now what?
Final answer above on Finalizing pleural effusion.
4 comments - CLICK HERE to read & add your own!:
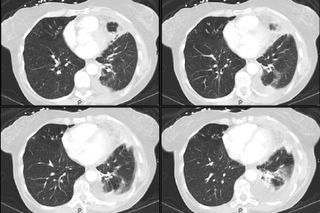
Now in contrast to the previous case, where MAC was likely a contaminant, I would personally treat the staph that you got from the bronch. It is indeed possible that she has staph pneumonia (although the infiltrate is small on the cuts you provided), with a complicated parapneumonic effusion. I dop not think she needs a chest tube per se, but I would give her a full course of vanco (or linezolid if home IV not convenient) and follow closely with repeat radiographs (CT at first to ensure resolution.
I agree with treating this as pneumonia. The results of the thoracentesis are not incompatible with this diagnosis. We can certainly see "much less lung" tissue on the left than on the right on the cuts provided. Besides there seems to be partial loculation and thickening of the pleura underneath the residual effusion. I would not abandon the thought about chest tube; I believe that she will likely need VATS/decortication as will likely cause significant restriction.
I also agree with treating. I can't say I definitely see pleural thickening, but it is certainly a loculated effusion. Decortication may be necessary down the line, but that will really depend on the degree of her residual (if any) dyspnea and functional impairment following treatment and a recovery period.
Quick answers to some of the comments so far: the soft-tissue windows did not add much: no adenopathy, no masses, those densities were all air-filling/parenchymal disease. We did not place a chest tube: the fluid was free-flowing, non-purulent and after re-tapping was almost all gone. Fluid Cxs remained negative.
We started vanco and she felt much better. I will post the final answers tomorrow.
Post a Commenttest post a comment