This is a 65 y/o previously healthy woman. No TOB, no chronic lung disease, no cardiac disease. She was transferred from an OSH with 2 weeks of low-grade fevers and now has a dry cough, orthopnea, worsening DOE and L pleuritic CP. No hemoptysis or purulent sputum production.
Unremarkable PMHx, SHx and FHx.
ROS + for chills and fevers, no night sweats. Resp as per HPI. No GI/GU complaints.
Her exam was mostly normal except for decreased BS, dullness to percussion and egophony on the L base.
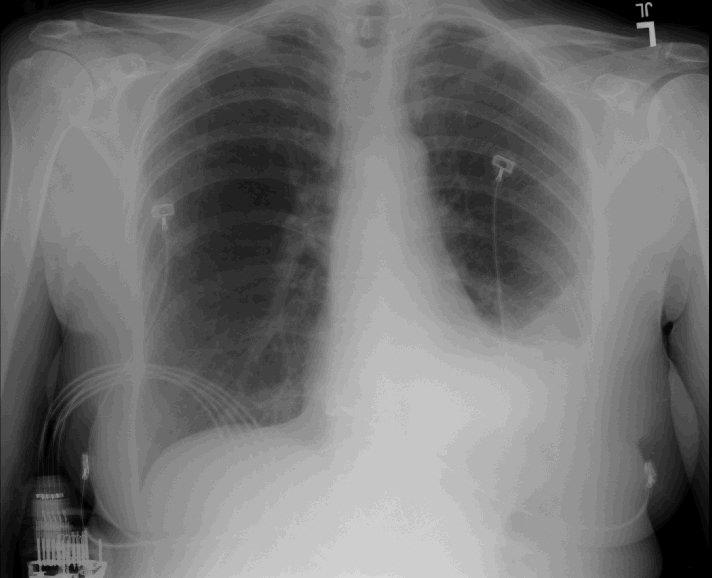
Her inital WBC count was 5K with aleft shift. Unfortunatelly her first CxR was an outside film so I can't post it: it showed a large L effusion (3/4s up). A thoracentesis was performed and post-tap CxR is as follows.
Her pleural fluid revealed: 24,440 WBCs (all Monos), LDH 1755 and glucose 65 with no organsims seen.
What would you do next and what is your DDx?
Follow-up above on Follow-up to Pleural Effusion.
Subscribe to:
Post Comments (Atom)
12 comments - CLICK HERE to read & add your own!:
Oh, BTW, cytology on the fluid was negative for malignancy.
What I find most striking about this is the large predominance of mononuclear cells in this exudative effusion. That reduces the liklihood of a bacterial infection. TB also seems less likely, as that should have a lymphocytic predominance. I suspect that this could be a lymphoma, and would repeat the tap and send it for flow-cytometry. I would also consider a pleural biopsy, as well as serial taps followed by a CT scan of the chest and abdomen.
I am trying to think of what causes a monocytic predominate effusion. At the least, it probably represents a chronic process. I agree this would make TB less likely, but not sure if it rules it out. I realize a PPD is only most useful for screening, not diagnosis, but was she ppd positive?
Autoimmune disorders with monocytes (chronic) might occur; her age makes this a bit less likely. In that vein, the glucose level pretty much rules out rheumatoid...
You have to think that monocytes go to the site in response to chemokines, much of which is produced by neutrophils and (later on), lymphocytes. So again I would not ignore things that traditionally give a lymphocytic-predominate effusion like TB and lymphoma (as pointed out by horowitz).
I certainly agree with all the above posts. I strongly suspect a lymphoma.
With that super elevated LDH, I may strongly consider throwing in a chest tube, and then obtain all samples that we need. A ct thorax after drainage will be of great help to rule out any parenchymal infiltrate (not unusual for lymphoma), and also any mediastinal lymphadenopathy. I wonder whether you checked the PH on the fluid, serum glucose...).
I after all the above we still don't have a diagnosis, I would get the thoracic surgeon on board for VATS.
It seems as if there is left lower lobe collapse/partial collapse, with volume loss. While an endobronchial lesion is also a possibility, that would not account for the LDH or WBC elevation in the fluid. I still would not do bronchoscopy at this time. that may come 4 or 5 steps down the road (after chest tube, redo fluid analysis, CT, +/- VATS...)
any splenic enlargment on physical?
I'm not sure I'd put in a chest tube at this time: we have no idea how quickly the pleural fluid is accumulating. If it is accumulating rapidly, we can get into trouble with a chest tube, as ongoing fluid loss can be very high, we may not be able to completely drain the pleural space, and we may then have trouble removing the chest tube.
I typically would like to have a diagnosis prior to chest tube placement, and would do serial large volume thoracenteses; these would give us all the fluid we need without the risks associated with a chest tube in these circumstances.
well, I am not convinced about the reasoning behind delaying the chest tube placement. Such a high LDH is very concerning, and unless drained adequately, you may end up with a trapped lung. This effusion is complicated by definition. We are not dealing here with a hepatic hydrothrax, with "benign looking fluid" filling up the lung as soon as you drain it. Ther are only few conditions that would give you such a high LDH, and none of them (whether infections or cancer) have an uncomplicated course. Besides, it is very likely that this patient will need biopsy with VATS (if the above workup is non diagnostic), in which situation she will need a chest tube.
The effusion has been present long enough that if there is trapped lung, it is already there. And that's exactly what I don't want to put a chest tube into. If there is trapped lung, and VATS is necessary, a decortication would need to be done at the same time. If a trapped lung is already there, a chest tube will be of no value in drainage, as the negative thoracic pressure will cause fluid to continue to fill the pleural space. There are plenty of studies, even in complicated pleural effusions, that serial thoracentesis are effective.
I see your point and acknowledge your concern. I am not opposed to serial thoracenteses, and in fact would have gone that route if the LDH was 1/2 to 1/3 of what it is here. I think the risk is high for complications without evacuation of the pleural space.
We don't have a "trapped lung" yet in this case based on the post thoracentesis CXR, but that may happen if we wait longer. On the other hand if you believe that already there is trapped lung, the fluid characteristics are not suggestive of that.
One thing additional I would do is check the chracteritics of the fluid to ensure that there is no concomitant chylothorax as lymphoma can cause that, and in that situation I would not put a chest tube.
Great case. Pleural disease is always tricky.
I would repeat the tap (as per the other responders) to see if any malignant cells are present. You can get up to 80% of malignant pleural effusions if you do 2-3 taps.
By definition, a monocyte predominent effusion is a chronic process. I would not place a chest tube as if the thoracic surgeons need to decorticate/biopsy, it creates more problems (at least according ot them). The only caveat to that would be if she clearly had antecedent pulmonary symptoms consistent with a pneumonia.
Before the 2nd tap, I would get a CT of the chest to see if there is anything else to help make a diagnosis.
Someone else please comment on JCH's suggestion of flow cytometry: my understanding is that it is helpful only in making a diagnosis of lymphoma; she has a monocyte predominent effusion.
Agreed. By serial thoracentesis, I mean three large volume taps separated by hours (not one tap a day for consecutive days). The goal is the same--drain as much as possible and then image the lung.
I've seen too many people get into trouble throwing in chest tubes in this kind of situation then not being able to remove the chest tube. Even in the case of malignant effusions, a pleurex catheter or pleurodesis usually becomes necessary. I think we can all agree that, right now, this is not an empyema.
I'm not sure what the fluid characteristics of "trapped lung" are. In this setting, I don't mean that the trapped lung is causing the effusion (i.e. negative-pressure induced transudate). Instead, my concern is that the patient has had an strongly exudative effusion for two weeks (at least), and there may very well be a component of fibrothorax, which would necessitate a decortication.
Post a Commenttest post a comment