This is a 54 y/o man with a 2-pack day TOB habit who had been referred to us for atypical chest pain. He complained of intermittent chest tightness and had had a negative cardiac w/up (normal SPECT-stress, normal EF, etc.). We identified a mild to moderate obstructive ventilatory deffect (normal FVC and FEV1 that fluctuated between high 50s to 70%) and started him on bronchodilators and continued to counsel him about smoking. He had a CxR with a RUL bulla and some L apical scarring. In the course of his follow-up however, we performed a repeat CxR which revealed a new LUL lesion:
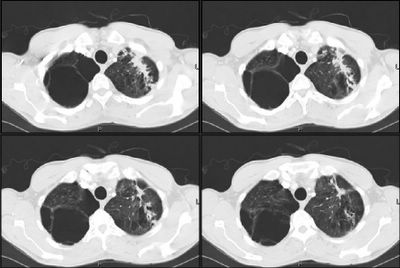
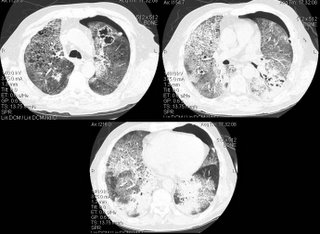
He had some cough at the time so he was given a course of ABTx and followed closely and there was no improvement in the lesion after 4 weeks. A CT scan was obtained and revealed a soft tissue mass associated with some scarring:
A bronch was done and was non-diagnostic and the mass remained unchanged on CxR.
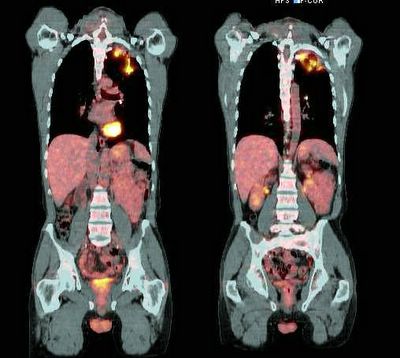
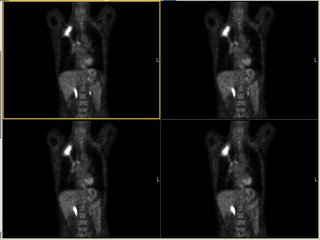
A PET-CT was then performed and revealed intense uptake on the area (SUV ~5.7 about 6 weeks after he had completed the course of ABTx) :
What would you do next?
Wednesday, November 30, 2005
Tuesday, November 29, 2005
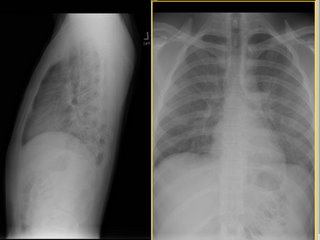
Abnormal CxR and hypoxemia
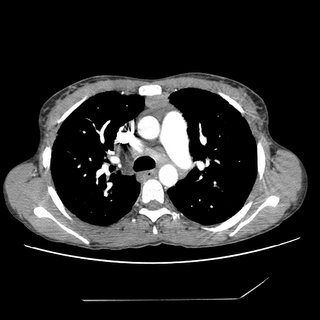
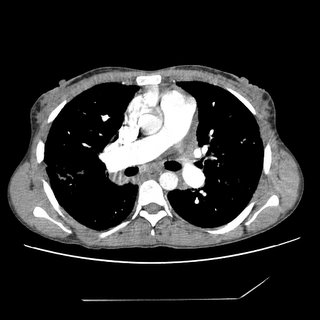
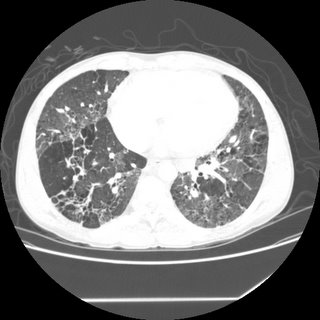
We were consulted on this pleasant 58-year-old white male with known coronary artery disease. He was last admitted 3 months ago with a inferior lateral wall myocardial infarction. He is status post angioplasty. He has a history of chronic obstructive pulmonary disease. He had been doing fairly well andhad gone back to work as an electrician however, over the last five days he developed increasing lethargy, chills and felt feverish with a dry nonproductive cough and worsening dyspnea.
PMHx: Ventricular tachycardia, S/P AICD/PM. CAD, S/P inferior lateral myocardial infarction and previous EF~45%. He is status post stenting of the OM/circumflex. Chronic obstructive pulmonary disease. Dyslipidemia.
Current meds: Lovenox, Albuterol and Atrovent, Levofloxacin, Aspirin and Amiodarone.
FHx: Noncontributory
SHx: Heavy cigarette smoker, he quit 3 months ago. He has been drinking several beers daily. He works as an electrician. He lives alone and his wife died last year.
ROS non-contributory.
On exam he was tachypneic to 36 with an O2Sat of 90% on BiPAP with 100% FiO2. BP and HR were stable. His lungs had very faint crackles and no wheezing or ronchi.
ABG was: 7.43/CO2: 37/ O2: 58 on 100% FM.
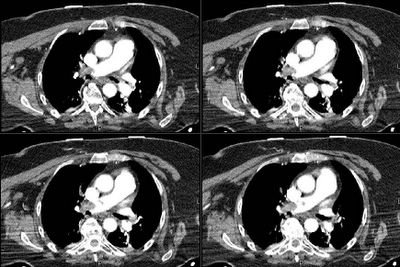
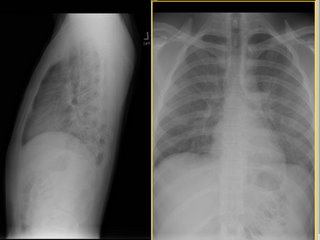
His CxR and CT are posted below.
What would you do next?
PMHx: Ventricular tachycardia, S/P AICD/PM. CAD, S/P inferior lateral myocardial infarction and previous EF~45%. He is status post stenting of the OM/circumflex. Chronic obstructive pulmonary disease. Dyslipidemia.
Current meds: Lovenox, Albuterol and Atrovent, Levofloxacin, Aspirin and Amiodarone.
FHx: Noncontributory
SHx: Heavy cigarette smoker, he quit 3 months ago. He has been drinking several beers daily. He works as an electrician. He lives alone and his wife died last year.
ROS non-contributory.
On exam he was tachypneic to 36 with an O2Sat of 90% on BiPAP with 100% FiO2. BP and HR were stable. His lungs had very faint crackles and no wheezing or ronchi.
ABG was: 7.43/CO2: 37/ O2: 58 on 100% FM.
His CxR and CT are posted below.
What would you do next?
Monday, November 28, 2005
ICS in COPD
This is a quick question. How often do you add inhaled steroids in the care of your COPD patients? I am more curious about people's anecdotal and personal opinions rather than data (FEV1< 30%, response to PO steroid trial, etc.).
Thursday, November 24, 2005
Tuesday, November 22, 2005
Follow-up to Picture Friday (Janeway lesions)
This is the 65 y/o man with FUO and palmar and plantar lesions. He has now had about 4 weeks of ABTx. His serologies for Coxiella and RMSF (and other Rickettsia) have been negative. His TEE showed some abnormal signal at one of his pacer leads but no vegetations. He remains afebrile, his Janeway lesions and splinter hemorrhages are almost completely gone and his arthralgias resolved. A Bx of one of his lesions was read as embolic infectious vasculitis. We still don't have an organism but with his good clinical response I have called it "culture-negative endovascular infection" and he will have a total of 6 weeks of therapy because of the hardware (PM). Any other ideas?
Monday, November 21, 2005
Consult to "bronch"
We were asked to consult on a patient to "rule out endobronchial lesion via bronch".
A 52-year-old male has an unremarkable past medical history. He has a 100 pack-year histor and is an alcoholic. He noticed a "boil" over his "right collar bone". He thought maybe he was bitten by an insect. Since then has had progressivesymptoms resulting in chest pain and difficulty breathing.
Blood pressure 120/70, heart rate 120, respiratory rate 22, temperature 36.4. 99% on four liters nasal cannula. General appearance: This is a cachectic male. Lungs sounds were significant for good air entry bilaterally with vesicular breath sounds, no rhonchi or wheeze appreciated. Cardiovascular significant for a tachycardia. otherwise unremarkable. b Over the mid sternum at around T3 is a 1 cm round red maculopapular lesion; no pus from the site.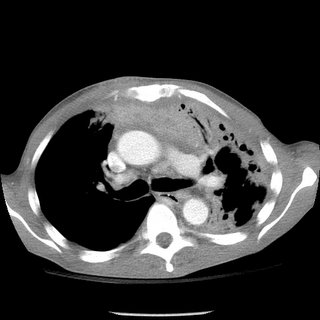

A 52-year-old male has an unremarkable past medical history. He has a 100 pack-year histor and is an alcoholic. He noticed a "boil" over his "right collar bone". He thought maybe he was bitten by an insect. Since then has had progressivesymptoms resulting in chest pain and difficulty breathing.
Blood pressure 120/70, heart rate 120, respiratory rate 22, temperature 36.4. 99% on four liters nasal cannula. General appearance: This is a cachectic male. Lungs sounds were significant for good air entry bilaterally with vesicular breath sounds, no rhonchi or wheeze appreciated. Cardiovascular significant for a tachycardia. otherwise unremarkable. b Over the mid sternum at around T3 is a 1 cm round red maculopapular lesion; no pus from the site.

Thursday, November 17, 2005
Cool films!
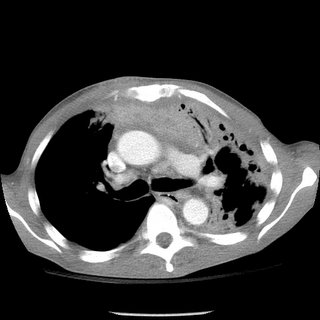
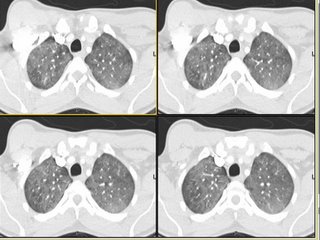
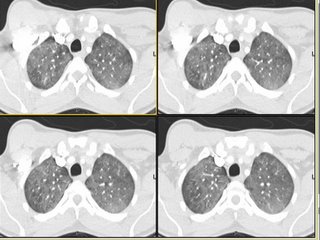
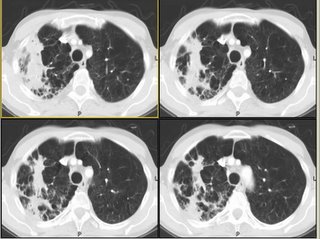
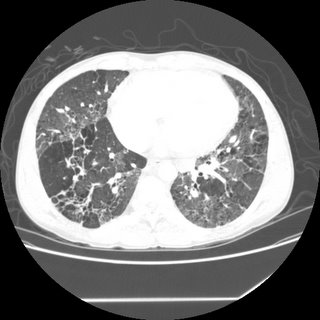
50-something y/o man with no significant past medical history prior to 3-4 months ago, when he developed progressive shortness of breath and required oxygen treatment. His evaluation elsewhere led to a diagnosis of BOOP on a surgical lung biopsy, and he was started on steroids-initially 20mg/day. He failed to improve, and a few weeks later his prednisone was bumped to 40mg/day, and then a few weeks later he had still failed to improve and his dose was increased to 60 mg/day.
A few weeks later, he was admitted to another hospital with continued dyspnea, and transferred to our institution, where he quickly developed respiratory distress. The following CT scan was obtained, and he was transferred to the ICU.
Questions:
1) What intervention led to a rapid improvement in this patients acute respiratory decompensation.
2) What is the the differential diagnosis for the other two findings on this CT scan
3) What steps would you take to further evaluate and treat the patient?
A few weeks later, he was admitted to another hospital with continued dyspnea, and transferred to our institution, where he quickly developed respiratory distress. The following CT scan was obtained, and he was transferred to the ICU.
Questions:
1) What intervention led to a rapid improvement in this patients acute respiratory decompensation.
2) What is the the differential diagnosis for the other two findings on this CT scan
3) What steps would you take to further evaluate and treat the patient?
Wednesday, November 16, 2005
Followup to 2 weeks of dyspnea
Mendez and Jeff H both picked up on the salient points. Here is the canned message from Carlos as he hangs out somewhere in Lima:
For those who picked up on the "clear lungs" with all the ground-glass we also suspected PCP in this young man with no other Hx of structural lung Dz. He was admitted at night so we started him on IV bactrim and steroids (and a 3 rd gen Cef), ordered a rapid HIV test and planned on doing a bronch. His HIV was positive and then they volunteered his partner was HIV+ and requested a transfer to a University Hospital here in TN. His PCP DNA PCR was positive, his CD4 was around 50 and overall he did very well. Here is his follow-up CxR:
For those who picked up on the "clear lungs" with all the ground-glass we also suspected PCP in this young man with no other Hx of structural lung Dz. He was admitted at night so we started him on IV bactrim and steroids (and a 3 rd gen Cef), ordered a rapid HIV test and planned on doing a bronch. His HIV was positive and then they volunteered his partner was HIV+ and requested a transfer to a University Hospital here in TN. His PCP DNA PCR was positive, his CD4 was around 50 and overall he did very well. Here is his follow-up CxR:

ARDS and pulmonary function
From a PCP in NC:
"Quick question: what PFT parameter is the last to normalize (if it ever does) in patients with ARDS, 1 year out?" The pulmonary boards were yesterday so some of you fellows out there should have no problem with this question.....
"Quick question: what PFT parameter is the last to normalize (if it ever does) in patients with ARDS, 1 year out?" The pulmonary boards were yesterday so some of you fellows out there should have no problem with this question.....
Tuesday, November 15, 2005
2 weeks of dyspnea
Carlos' case:
We were consulted on this is a 28 y/o man with no previous PMHx who presented to the ER with progressive worsening DOE over the past 2-3 weeks with some dry cough. Occasional chills but no fevers or night sweats. In the ER he was febrile and hypoxic (7.47/33/58) and was admitted for further care.
PMHx: No lung Dz.
SHx: Occasional ETOH, TOB 1ppd x 10 years, no occupational exposures, no IVDA, lives with same-sex partner.
On exam, AAOx3 in minimal resp discomfort. Clear lungs B/L. S1/S2 RRR and benign abdomen.
CxR:
The ER did a CT-angio (on everybody), which showed no PE but the following changes:
What is your DDx and what would you do next?
We were consulted on this is a 28 y/o man with no previous PMHx who presented to the ER with progressive worsening DOE over the past 2-3 weeks with some dry cough. Occasional chills but no fevers or night sweats. In the ER he was febrile and hypoxic (7.47/33/58) and was admitted for further care.
PMHx: No lung Dz.
SHx: Occasional ETOH, TOB 1ppd x 10 years, no occupational exposures, no IVDA, lives with same-sex partner.
On exam, AAOx3 in minimal resp discomfort. Clear lungs B/L. S1/S2 RRR and benign abdomen.
CxR:
The ER did a CT-angio (on everybody), which showed no PE but the following changes:
What is your DDx and what would you do next?
Monday, November 14, 2005
Pulmonary embolism and intervention
The cover of the Nov 1st Blue journal (AJRCCM 172(9)) showing a fibrosed thrombus reminded me how controversial treatment of this entity can be. I was interested in what others felt about the following. We all know that no study has demonstrated a change in mortality after thrombolytic therapy for acute massive PE. We also know that some of the beneficial paramters (such as right heart strain or PA pressure) are no different than just IV heparin after about 7 days. Nonetheless, does anyone feel that the lack of a mortality benefit may be as a result of the studies being underpowered? If this is the case, perhaps thrombolytics should be used as default pending a larger study (for massive PE without obvious bleeding risks). On the other hand, if the concensus is that nothing is proven with regards to mortality and thus thrombolytics are NOT indicated by default until that larger study comes along, should we ever administer it?
Now it gets even more sketchy when we consider surgical embolectomy. When do you consider this intervention? Some have argued that it absolutely has no place. Others will ship everyone with a b/l saddle embolus out to the Mayo for embolectomy.
I think there is not a lot of convincing data out there for anything other than good old fashioned anticoagulation and IV fluids (and some prayer).
What do you all do when you get the call about a patient with acute massive P.E.?
Now it gets even more sketchy when we consider surgical embolectomy. When do you consider this intervention? Some have argued that it absolutely has no place. Others will ship everyone with a b/l saddle embolus out to the Mayo for embolectomy.
I think there is not a lot of convincing data out there for anything other than good old fashioned anticoagulation and IV fluids (and some prayer).
What do you all do when you get the call about a patient with acute massive P.E.?
Sunday, November 13, 2005
When to Treat MAI
80 yo female with PVOD s/p TIA many years ago presented with multiple pulm nodules about 2 years ago to her PCP. The radiologist was worried about TB at the time, so she was sent to the county health clinic. The CT also showed evidence of broniectasis at that time. Sputum cultures revealed MAI.
She went to an ID doc, who convinced her the treatment is worse than the disease. So, she opted for no treatment.
She is pretty much asymptomatic since 1/04 (the time of her original CT), but she presented to the ER with hemoptysis (about 5 tbsp, bloody sputum with clots). She was watched in observation overnight and it did not recur.
Her repeat CT scan (to rule out PE, of course), showed stable nodules. There were more of them, but the ones visualized 2 years ago are definitively stable.

Would you offer a bronch, or is the CT with bronchiectasis enough to convince you of the diagnosis (she has never before been endoscopically evaluated)?
Would you treat the MAI in this 80 yo, relatively asymptomatic individual?
She went to an ID doc, who convinced her the treatment is worse than the disease. So, she opted for no treatment.
She is pretty much asymptomatic since 1/04 (the time of her original CT), but she presented to the ER with hemoptysis (about 5 tbsp, bloody sputum with clots). She was watched in observation overnight and it did not recur.
Her repeat CT scan (to rule out PE, of course), showed stable nodules. There were more of them, but the ones visualized 2 years ago are definitively stable.

Would you offer a bronch, or is the CT with bronchiectasis enough to convince you of the diagnosis (she has never before been endoscopically evaluated)?
Would you treat the MAI in this 80 yo, relatively asymptomatic individual?
Tuesday, November 08, 2005
COPD and weight loss.
From Carlos, who is on vacation:
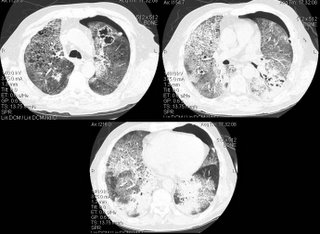
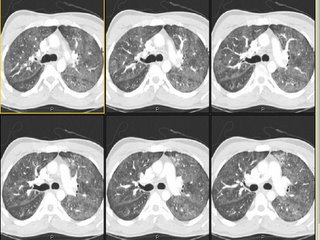
This is a 60 y/o man with a 50 p/y Hx of smoking sent to us because of worsening DOE, cough productive of scant amounts of thick sputum and weight loss. No hemoptysis, no CP.
PMHx: Mild HTN.
SHx: 50 p/y TOB. Quit in 2003.
On exam, thin male in NAD. Distant BS B/L with rare R upper crackles. S1/S2 RRR, benign abdomen.
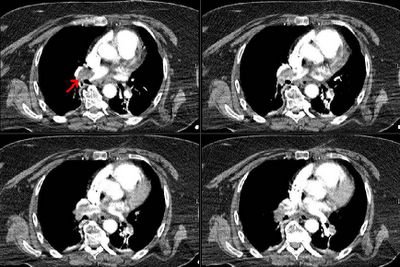
His Spiro revealed an FEV1 of 1.1 L (27% of his predicted) and he had the following CxR and CT scan findings:

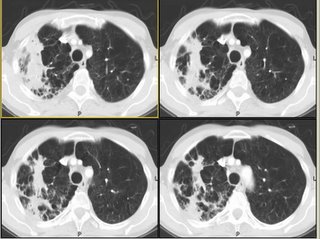
update(after 1st 2 comments):
He was started on aggressive bronchodilator therapy, given ABTx and steroids and returned with symptomatic improvement. His FEV1 increased to 2.17L (53%) and he felt better. However, he still had some weight loss (6 lbs.) and a persistent infiltrate after 4 weeks. I did a bronch which revealed only chronic bronchitis and no other Dx.
A PET-CT was done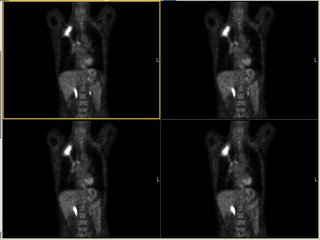 and it revealed marked FDG uptake to the RUL (average SVU of 13 with max SVU of 21) and nowhere else. What would you do next?
and it revealed marked FDG uptake to the RUL (average SVU of 13 with max SVU of 21) and nowhere else. What would you do next?
This is a 60 y/o man with a 50 p/y Hx of smoking sent to us because of worsening DOE, cough productive of scant amounts of thick sputum and weight loss. No hemoptysis, no CP.
PMHx: Mild HTN.
SHx: 50 p/y TOB. Quit in 2003.
On exam, thin male in NAD. Distant BS B/L with rare R upper crackles. S1/S2 RRR, benign abdomen.
His Spiro revealed an FEV1 of 1.1 L (27% of his predicted) and he had the following CxR and CT scan findings:

update(after 1st 2 comments):
He was started on aggressive bronchodilator therapy, given ABTx and steroids and returned with symptomatic improvement. His FEV1 increased to 2.17L (53%) and he felt better. However, he still had some weight loss (6 lbs.) and a persistent infiltrate after 4 weeks. I did a bronch which revealed only chronic bronchitis and no other Dx.
A PET-CT was done
 and it revealed marked FDG uptake to the RUL (average SVU of 13 with max SVU of 21) and nowhere else. What would you do next?
and it revealed marked FDG uptake to the RUL (average SVU of 13 with max SVU of 21) and nowhere else. What would you do next?
Monday, November 07, 2005
18 year old with hemoptysis
18-year-old male referred for hemoptysis. He reports several episodes of pneumonia in last several years. His mother believes that these have all been on the "right chest." The most recent episode of pneumonia had occurred during the last football season, when he developed cough and hemoptysis. By report, he had an abnormal chest x-ray at that time. He was treated with antibiotics and reports that the symptoms resolved. He again had hemoptysis in a few months later. A PPD was negative. No images of a chest CT, but there was right middle lobe bronchiectasis.
Pmhx Status post hernia repair, rhinoplasty, right elbow surgery. In addition, the patient has a history of a racing heart and has been worked up for possible supraventricular tachycardia. In addition, the patient had a mole punch biopsied off his left back inferior to the scapula and does not know what the pathology for this showed.
SH: no alcohol, tobacco, or drug use
Physical Exam: His P is 49. BP is 108/57. His RR is 16, and his WT is 79 kg. In appearance, he is a well-developed, well- nourished young man in no distress. HEENT: Lymph node examination was no supraclavicular adenopathy. Pulmonary: clear to auscultation with both quiet and forced expiratory maneuvers from base to apex bilaterally. He is resonant to percussion throughout. Cardiac examination: Regular rhythm. S1 and S2 are of normal quality without murmur, gallop, or rub. He had no pedal edema, and he had 2+ radial pulses.
A bronch showd the following in the RML:
My collegue proceeded to evaluate further into the bronchus where they identified copious mucous and a foreign body. The foreign body was extracted with biopsy forceps. Under direct visualization it appeared to be a piece of organic green matter that resembled a branch tip of a pine tree.
Final diagnosis:
LUNG, RIGHT MIDDLE LOBE, BIOPSY:
1. BENIGN MARKEDLY INFLAMED BRONCHIAL MUCOSA AND FRAGMENTS OF
GRANULATION TISSUE.
2. FOREIGN MATERIAL CONSISTENT WITH VEGETABLE PARTICLE.
B. RIGHT LOBE, BIOPSY: FOREIGN BODY.
The patient breathed in a pine needle....
Pmhx Status post hernia repair, rhinoplasty, right elbow surgery. In addition, the patient has a history of a racing heart and has been worked up for possible supraventricular tachycardia. In addition, the patient had a mole punch biopsied off his left back inferior to the scapula and does not know what the pathology for this showed.
SH: no alcohol, tobacco, or drug use
Physical Exam: His P is 49. BP is 108/57. His RR is 16, and his WT is 79 kg. In appearance, he is a well-developed, well- nourished young man in no distress. HEENT: Lymph node examination was no supraclavicular adenopathy. Pulmonary: clear to auscultation with both quiet and forced expiratory maneuvers from base to apex bilaterally. He is resonant to percussion throughout. Cardiac examination: Regular rhythm. S1 and S2 are of normal quality without murmur, gallop, or rub. He had no pedal edema, and he had 2+ radial pulses.
A bronch showd the following in the RML:

My collegue proceeded to evaluate further into the bronchus where they identified copious mucous and a foreign body. The foreign body was extracted with biopsy forceps. Under direct visualization it appeared to be a piece of organic green matter that resembled a branch tip of a pine tree.
Final diagnosis:
LUNG, RIGHT MIDDLE LOBE, BIOPSY:
1. BENIGN MARKEDLY INFLAMED BRONCHIAL MUCOSA AND FRAGMENTS OF
GRANULATION TISSUE.
2. FOREIGN MATERIAL CONSISTENT WITH VEGETABLE PARTICLE.
B. RIGHT LOBE, BIOPSY: FOREIGN BODY.
The patient breathed in a pine needle....
Friday, November 04, 2005
Approach to this lesion
A physician wants some feedback regarding how to approach this lesion. This is an abdominal CT. A chest CT has not yet been done. The quesion regarding approach: get a PET? Go right to CT-guided biopsy? Get a full CT of chest first in case soemthign shows up that would make a bronch more helpful?
He's a patient with COPD and heavy smoking history. Abd CT was obtained b/c of some nausea.

He's a patient with COPD and heavy smoking history. Abd CT was obtained b/c of some nausea.

Thursday, November 03, 2005
Check out our ongoing cases!
Just a reminder to check on some of the ongoing cases.
DKeena had a great case on Enbrel-associated infiltrates in need of comments.
I have posted follow-ups to the drop in ETCO2 case (check out the CT) and the abnormal CxR as well as the presumed IE.
And we are looking forward to more info on Jennings' case with pancytopenia and abnormal lungs.
DKeena had a great case on Enbrel-associated infiltrates in need of comments.
I have posted follow-ups to the drop in ETCO2 case (check out the CT) and the abnormal CxR as well as the presumed IE.
And we are looking forward to more info on Jennings' case with pancytopenia and abnormal lungs.
Update on "update on picture Friday"
This is the 65 y/o man with FUO and palmar and plantar lesions posted on Picture Friday. There have been a few very good new comments on the original post. Dr Jon wrote:
Rickettsial infection: what about R. prowazekii? More common in elderly, and consistent with petechiae, but not common in US. Has he ever had typhus? There is Brill-Zinsser Disease (has he ever traveled outside th country?)Also about the endocarditis, maybe C. psittaci (hard/impossible to culture), does he have any birds?
He did not have birds and no exposures to suggest typhus. No recent travels. His serologies for Q fever, RMSF, Rickettsia prowazekii and Ehrlichia came back today and were all negative. He has remained afebrile and his Janeway lesions are resolving. A skin punch biopsy was interpreted as infectious embolic vasculitis though no organisms were seen. All Cxs remain negative. A TEE showed no veggies but there were some echo changes at the PM atrial lead site concerning for a small endocardial abcess. His CRP is down from 30 to 6 but now his Creatinine has crept up from <1.5>3%.
So we are still treating him for Cx- IE. Any other ideas?
Rickettsial infection: what about R. prowazekii? More common in elderly, and consistent with petechiae, but not common in US. Has he ever had typhus? There is Brill-Zinsser Disease (has he ever traveled outside th country?)Also about the endocarditis, maybe C. psittaci (hard/impossible to culture), does he have any birds?
He did not have birds and no exposures to suggest typhus. No recent travels. His serologies for Q fever, RMSF, Rickettsia prowazekii and Ehrlichia came back today and were all negative. He has remained afebrile and his Janeway lesions are resolving. A skin punch biopsy was interpreted as infectious embolic vasculitis though no organisms were seen. All Cxs remain negative. A TEE showed no veggies but there were some echo changes at the PM atrial lead site concerning for a small endocardial abcess. His CRP is down from 30 to 6 but now his Creatinine has crept up from <1.5>3%.
So we are still treating him for Cx- IE. Any other ideas?
Follow-up to abnormal CxR - part II
This is the woman in her 70s with an abnormal CxR. After the thoracentesis she had more L lung collapse: by the time of the bronch and the f/up PET she had complete L lung collapse (making her at least a IIIA). Her past showed uptake only in the peri-hilar mass itself. Our surgeons and a CT surgeon from a large University Center nearby felt that though she was a IIIA, her lesion was very proximal (less than 2 cm to the carina) and she would be a poor candidate for a pneumonectomy so she is receivin Chemo and xRt. She will follow-up with us and may benefit from APC or stenting to the lesion to improve drainage/clearance of the collapsed lung.
Wednesday, November 02, 2005
Unbound Medicine
We came across this jewel of a site from Mexico that focuses on medical education. As such there are some interesting cases posted there.
Follow-up to abnormal CxR
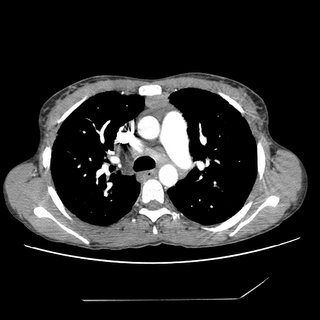
This is the woman in her 70s with an abnormal CxR. Everyone picked up on the loss of volume and nobody was "fooled" by the negative CT last year (it was really unremarkable). She had a CT scan seen below:
Most of her L lung was collapsed with a smallish effusion. Her effusion was exudative with negative cytology. I did a bronch and she had a NSCLCa occluding her L mainstem bronchus. Her Spiro (with her L lung collapsed) revealed an FEV1~ 800cc.
What would you suggest as the next step?
Most of her L lung was collapsed with a smallish effusion. Her effusion was exudative with negative cytology. I did a bronch and she had a NSCLCa occluding her L mainstem bronchus. Her Spiro (with her L lung collapsed) revealed an FEV1~ 800cc.
What would you suggest as the next step?
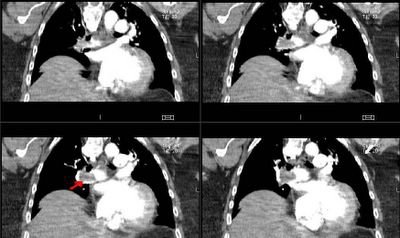
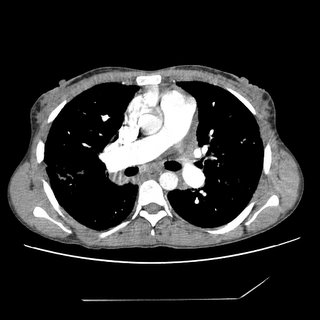
Follow-up to drop in ETCO2
Good comments on this case. A drop in ETCO2 suggests a massive mismatch or loss of pulmonary vascular perfusion. Cardiac arrest would do that but I did not describe full arrest. DKeena mentioned esophageal intubation. It can be tricky especially in emergencies when a lot or air is bagged into the stomach and an initially +ETCO2 drops as the tube stays in the esophagus. Massive PE will cause a decrease in CO2-rich blood flow to the lungs. Since her ETT was properly placed and her EKG showed no ischemic changes (just the LAFB) and she is a sedentary (having back surgery, remmember?) I was concerned she had had a PE and requested and emergent CT. Check it out below:
Would you thrombolyze her?
What would you do next?
Would you thrombolyze her?
What would you do next?
Tuesday, November 01, 2005
Quick follow-up to Asthma (with Strongyloides)
This is the 20 y/o woman with bronchospasm and cough after her missionary trips. She has finished her course of Albendazole and has been on Asmanex (mometasone). She is now assymptomatic, her lungs are completely clear and her FEV1 increased from 2.29L(76%) to 3.30L(110%) and her ratio increased from 80% to 87%. We are weaning her Asmanex off and her repeat stool O&P were negative.
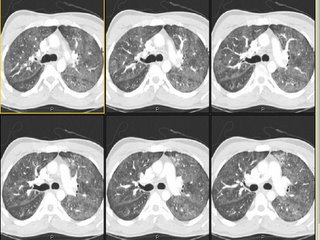
Pancytopenia, abnormal cxr
I hope to have a lively debate because there is some controversy about the following case:
34 y/o AA woman with pancytopenia 10 years ago. Asymptomatic, lost to f/u because of insurance. Refused BM biopsy. 5 years ago gradual onset of dyspnea. May of this year presented with SOB and admitted. (Pulmonary consult called at that time). On exam she had some JVD, clear lungs, loud O2, hepatosplenomegaly, ascites and 2+ pitting edema. Echo showed PAP of 48 with dilated RV and an LV with an EF of 65%. Labs: WBS 2.2 with 82% N, Hgb 9, plts 104. ACE was 207.
CXR and CT:


Bronch BAL not sent, therefore cell count and micro of the fluid unknown. A TBBX showed of the RNL showed a single poorly formed granuloma. The micro on the biopsy *was* sent and was negative. Endobronchial biopsy showed active chronic inflammation.
Urinary histo Ag never sent. Serum Ab's against fungus also not sent.
Questions:
1. Would you consider the above info sufficient stop at the diagnosis of sarcoid?
2. Would you be satisfied with no infectious cause based on negative Tbbx micro, but BAL not sent?
3. Do you feel that a cell count with CD4 and CD8 would have been helpful to you?
4. (corollary to 1): Is there anything else on your differential list besides sarcoid? The person presenting this case to me has no other diagnoses on his list.
5. Does the history of 10 years of pancytopenia rule out histoplasmosis or other fungus?
34 y/o AA woman with pancytopenia 10 years ago. Asymptomatic, lost to f/u because of insurance. Refused BM biopsy. 5 years ago gradual onset of dyspnea. May of this year presented with SOB and admitted. (Pulmonary consult called at that time). On exam she had some JVD, clear lungs, loud O2, hepatosplenomegaly, ascites and 2+ pitting edema. Echo showed PAP of 48 with dilated RV and an LV with an EF of 65%. Labs: WBS 2.2 with 82% N, Hgb 9, plts 104. ACE was 207.
CXR and CT:



Bronch BAL not sent, therefore cell count and micro of the fluid unknown. A TBBX showed of the RNL showed a single poorly formed granuloma. The micro on the biopsy *was* sent and was negative. Endobronchial biopsy showed active chronic inflammation.
Urinary histo Ag never sent. Serum Ab's against fungus also not sent.
Questions:
1. Would you consider the above info sufficient stop at the diagnosis of sarcoid?
2. Would you be satisfied with no infectious cause based on negative Tbbx micro, but BAL not sent?
3. Do you feel that a cell count with CD4 and CD8 would have been helpful to you?
4. (corollary to 1): Is there anything else on your differential list besides sarcoid? The person presenting this case to me has no other diagnoses on his list.
5. Does the history of 10 years of pancytopenia rule out histoplasmosis or other fungus?
Subscribe to:
Comments (Atom)