We were consulted on this is a 28 y/o man with no previous PMHx who presented to the ER with progressive worsening DOE over the past 2-3 weeks with some dry cough. Occasional chills but no fevers or night sweats. In the ER he was febrile and hypoxic (7.47/33/58) and was admitted for further care.
PMHx: No lung Dz.
SHx: Occasional ETOH, TOB 1ppd x 10 years, no occupational exposures, no IVDA, lives with same-sex partner.
On exam, AAOx3 in minimal resp discomfort. Clear lungs B/L. S1/S2 RRR and benign abdomen.
CxR:

The ER did a CT-angio (on everybody), which showed no PE but the following changes:

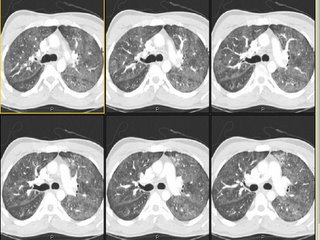
What is your DDx and what would you do next?
1 comments - CLICK HERE to read & add your own!:
I think Mendez has hit this one on the head. Only things I'd add at this point: sputum for PCP, and a UA to look for red-cell casts. My top two on the differential for this CT are PCP (although I don't see any cystic lesions), and acute HP (unclear exposure history).
Post a Commenttest post a comment