IS:
This is not a case presentation, but want to take a poll on what people are doing about steroids and sepsis. Do you administer steroids emperically after initial fluid bolus or do you attempt resuscitation per the 6hr bundle first and then administer steroids if still on pressors or hypotensive?
Friday, September 29, 2006
Tuesday, September 26, 2006
Follow-up to Anti-GM-CSF
I had posted this question but had no takers so I am posting a suggested answer. The Cleveland Clinic has an (investigational) Anti-GM-CSF autoantibody kit available for primary PAP. Check out this link for more info.
fluid filled lesion
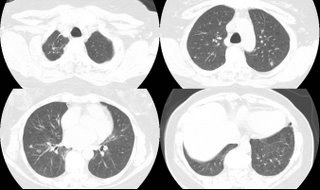
Update on Mass and Infiltrates
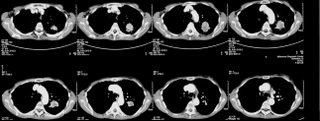
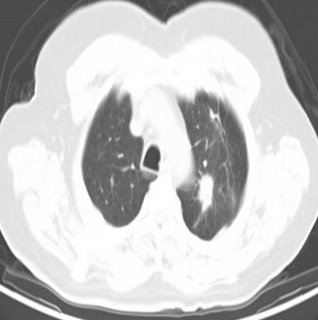
I had posted on this 59 y/o woman with a funny presentation: she had had an episode of syncope at home, hit her head and had a skin lac requiring 7 stitches. While being worked up in the ER they found her to be hypotensive and febrile with an abnormal CxR and CT of the chest. She had MSSA in her sputum and a dense lung "mass". I bronch'ed her and got "organizing pneumonia" but no malignancy. She got ABTx and the "mass" went away completely. She did however had persistent smallish alveolar infiltrates seen below:

I re-bronched her focusing on the infiltrates since they had persisted for 3 months after the initial presentation. She had a lot of eosinophilic proteinaceous alveolar material and our pathologists sent the tissue to T. Colby who thought this was PAP.
Would you be satisfied with this Dx on TBBx or would you pursue an OLBx?
How about testing for anti-GM-CSF Antibodies?
She has almost normal lung function, how would you treat her?

I re-bronched her focusing on the infiltrates since they had persisted for 3 months after the initial presentation. She had a lot of eosinophilic proteinaceous alveolar material and our pathologists sent the tissue to T. Colby who thought this was PAP.
Would you be satisfied with this Dx on TBBx or would you pursue an OLBx?
How about testing for anti-GM-CSF Antibodies?
She has almost normal lung function, how would you treat her?
Hemodynamics
A patient intubated and sedated for hypoxia (history of aspiration although CXR negative) had initial swan numbers of: CO 5 L, CI 3.24 PAP 26/16. PCW 8 with cvp of 4. SVR 1362. PVR is 190. AFter fluid boluses with no change in CO, PCW still 8 with a CVP of 6. His SBP has been 116/78 basically unchanged throughout. After fluid blouses he is now about 10 L up with really no change in the above swan readings or bloodpressure. How would you interpret this? Of note a surface echo showed an EF of 25-35%.
Here's his cxr.

Here's his cxr.

Thursday, September 21, 2006
Anti-GM-CSF antibodies
Have you been checkin anti-GM-CSF antibodies for evaluation of suspected PAP? If so, is there a commercially available ELISA or have you been sending those to the Cleveland Clinic?
Monday, September 18, 2006
Follow-up to Pulmonary-thyroid
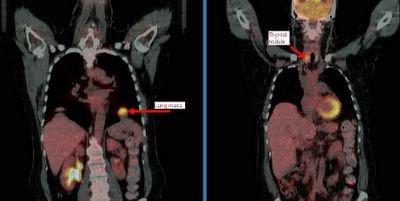
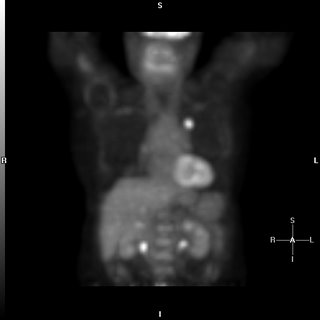
This is the patient with the hot pulmonary nodule and lung mass.
We decided to start with the thyroid and a bronch. The thyroid mass (it was not cystic on CT) was a follicular carcinoma with local invasion. No lymphnodes and the other lobe was clean.
The bronch was non-diagnostic and radiology felt the mass was too low and there was too much lung in its way for a good CT-guided needle.
She went to see our CT surgeons and we figured out why the bronch was non-diagnostic: it was not a lung mass but a diaphragmatic mass. It was an aneuploid adenomatoid tumor still not clearly characterized. Incidentally, there was a second focus of this same adenomatoid tumor in the superior segment of that LLL, which had not been seen on CT or PET (at ~7mm).
What do you think?
We decided to start with the thyroid and a bronch. The thyroid mass (it was not cystic on CT) was a follicular carcinoma with local invasion. No lymphnodes and the other lobe was clean.
The bronch was non-diagnostic and radiology felt the mass was too low and there was too much lung in its way for a good CT-guided needle.
She went to see our CT surgeons and we figured out why the bronch was non-diagnostic: it was not a lung mass but a diaphragmatic mass. It was an aneuploid adenomatoid tumor still not clearly characterized. Incidentally, there was a second focus of this same adenomatoid tumor in the superior segment of that LLL, which had not been seen on CT or PET (at ~7mm).
What do you think?
Friday, September 15, 2006
Wednesday, September 13, 2006
The pulmonary-thyroid connection

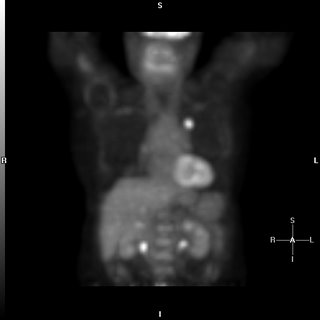
This patient came to me pre-worked up so I will show all the data she had had thus far. This is a 65 y/o woman with no TOB Hx, normal PFTs who had a persistent cough. She had an abnormal CxR (see above) and here PCP ordered a CT and then a PET-CT and she was sent to us.
Her PET scan showed two very FDG-avid lesions. A L basilar lung lesion and a R thyroid nodule with no other abnormal uptake. She is euthyroid clinically and by TFTs.
Do you think the lesion are related?
Would you biopsy one, the other, both?
Tuesday, September 12, 2006
LUL lesion, still undiagnosed
70 year old woman with COPD FEV1 34% predicted, but she is well compensated and on no supplemental oxygen (91% on RA). A LUL lesion was noted (see below) and workup included 2 bronchs (one with ultrasound-guided) and 1 CT-guided biopsy. All were negative for malignant cells. BAL was not done but Tbbx showed Atypical lymphoid cell with acute inflammation and Filamentous bacteria. BAL was not sent so we don't have micro ID (the bacteria was identified by path).
Cancer is obviously still number one on the list, but I dont think she's a surgical candidate and in terms of treating with chemo, we still dont have a tissue diagnosis. On the other hand, the filamentous bacteria finding is interesting. What is your impression and what would you all do next? Thanks.
Cancer is obviously still number one on the list, but I dont think she's a surgical candidate and in terms of treating with chemo, we still dont have a tissue diagnosis. On the other hand, the filamentous bacteria finding is interesting. What is your impression and what would you all do next? Thanks.
Monday, September 11, 2006
Bloody effusion
57 y/o man former smoker, presented with pleuritic CP and found to have left loculated effusion. No constitutional sx. no wt loss, fever, chills, cough. Tap 2 weeks later showed it to be bloody, with 57 WBC, 49% PMN and 49% lymphocytes. He is currently asymptomatic.
The effusion was AFB - times 1. The micro and cytology was negatrive. Dopplers of legs negative and V/Q was intermediate or indeterminate (cant remember) and PE-protocol CT was read as negative.
His Pmhx not remarkable except for 2 previous pneumonias. Last was in march and was on the right side. There was a small parapneumonic effusion which has since resolved.
No history of trauma except moving his furniture 1 day before the pleuritic CP, but he did not hit anything per se. No Fmhx of thrmbosis and in fact his Wells criteria is zero.
What would you all do next?
The effusion was AFB - times 1. The micro and cytology was negatrive. Dopplers of legs negative and V/Q was intermediate or indeterminate (cant remember) and PE-protocol CT was read as negative.
His Pmhx not remarkable except for 2 previous pneumonias. Last was in march and was on the right side. There was a small parapneumonic effusion which has since resolved.
No history of trauma except moving his furniture 1 day before the pleuritic CP, but he did not hit anything per se. No Fmhx of thrmbosis and in fact his Wells criteria is zero.
What would you all do next?
Thursday, September 07, 2006
Advice on further workup for this lung cancer.
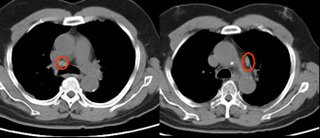
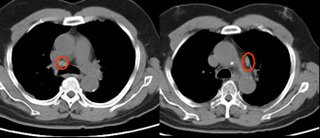
59 year old ex-smoker with FEV1 1.17 liters (47% predicted) who has a left upper lobe lesion:
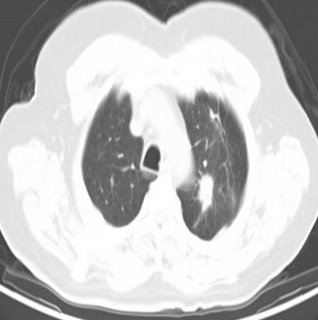
He also has some enlarged nodes (red circles):
The PET showed intense uptake of the LUL lesion and "mild hypermetabolic activity in the right hilar and pericarinal regions corresponding to nonenlarged lymph nodes on CT. This is of uncertain clinical significance. No other foci of abnormal hypermetabolic activity are identified.":
However, because of the enlarged nodes and the equivocal uptake on PET , I elected to sample them anyway;
The results showed no malignancy from the fine needle aspirate (but there were lymphocytes indicating that the node was sampled.
Not surprisingly, biopsy of the peripheral lesion in the LUL lesion was indeed cancer - adenocarcinoma.
Would you call this cancer a stage I (tumor was 2.4 x 1.4 cm) and proceed to surgery?
He also has some enlarged nodes (red circles):
The PET showed intense uptake of the LUL lesion and "mild hypermetabolic activity in the right hilar and pericarinal regions corresponding to nonenlarged lymph nodes on CT. This is of uncertain clinical significance. No other foci of abnormal hypermetabolic activity are identified.":
However, because of the enlarged nodes and the equivocal uptake on PET , I elected to sample them anyway;
The results showed no malignancy from the fine needle aspirate (but there were lymphocytes indicating that the node was sampled.
Not surprisingly, biopsy of the peripheral lesion in the LUL lesion was indeed cancer - adenocarcinoma.
Would you call this cancer a stage I (tumor was 2.4 x 1.4 cm) and proceed to surgery?
Wednesday, September 06, 2006
Multiple pulmonary nodules
The patient is a 69-year-old African-American woman who came to pulmonary clinic for multiple pulmonary nodules that were picked up in the course of abdominal CT for workup for abdominal pain with increased LFTs (which have since normalized). She has a history of hypertension, diabetes, peripheral vascular disease, and hyperlipidemia. She is a nonsmoker. No fever chills cough SOB, diaphoresis or constitutional symptoms.
Exam: A pleasant woman in no acute distress. WT of 197, BP 185/83, P is 65, R 18, O2 sat is 97% on room air. Trachea midline. No lymphadenopathy and no supraclavicular adenopathy. No thyromegaly. Lungs: Clear to auscultation. No wheezing, rales, or rhonchi. No dullness to percussion. No egophony, symmetric chest wall on inspiration. Heart: Regular rate. S1, S2. Abdomen: Positive bowel sounds. No masses. No liver edge felt. No clubbing, cyanosis, or edema.
Data:
PFT's: FEV1/FVC 81, FEV1 76% predicted, FVC 73% predicted.
CBC with hemoglobin of 10.3, MCV of 94.6. Plts normal. Lytes-7 normal. ANA and rheumatoid factor negative
These nodules are all non-calcified. The largest is 8 mm. There is interval growth of left lower lobe nodule and right apical nodule compared to a CT 6 months prior. The subcarinal soft tissue is "prominent" but ambiguous whether it's enlarged.
On abd CT, the spleen, pancreas, kidney, gallbladder and adrenals are unremarkable.
2 calcified hepatic granulomas are seen.
Any thoughts on workup or management?
.
Exam: A pleasant woman in no acute distress. WT of 197, BP 185/83, P is 65, R 18, O2 sat is 97% on room air. Trachea midline. No lymphadenopathy and no supraclavicular adenopathy. No thyromegaly. Lungs: Clear to auscultation. No wheezing, rales, or rhonchi. No dullness to percussion. No egophony, symmetric chest wall on inspiration. Heart: Regular rate. S1, S2. Abdomen: Positive bowel sounds. No masses. No liver edge felt. No clubbing, cyanosis, or edema.
Data:
PFT's: FEV1/FVC 81, FEV1 76% predicted, FVC 73% predicted.
CBC with hemoglobin of 10.3, MCV of 94.6. Plts normal. Lytes-7 normal. ANA and rheumatoid factor negative
These nodules are all non-calcified. The largest is 8 mm. There is interval growth of left lower lobe nodule and right apical nodule compared to a CT 6 months prior. The subcarinal soft tissue is "prominent" but ambiguous whether it's enlarged.
On abd CT, the spleen, pancreas, kidney, gallbladder and adrenals are unremarkable.
2 calcified hepatic granulomas are seen.
Any thoughts on workup or management?
.
Tuesday, September 05, 2006
Pulmonologist with high IgE
At ATS there was a stand on a rapid IgE testing system on capillary blood and some of us had it done just to check out the system.
One of us (with Hx of rhinitis but noasthma) had the results come back at an IgE level of 900 (their upper limit was 136).
Would you investigate it any further (CBC with diff, etc.) ?
One of us (with Hx of rhinitis but noasthma) had the results come back at an IgE level of 900 (their upper limit was 136).
Would you investigate it any further (CBC with diff, etc.) ?
Subscribe to:
Posts (Atom)