Past medical history: hypertension and moderate left ventricular hypertrophy seen on an echocardiogram, but negative cardiac stress test.
SOCIAL HISTORY: She is a lifelong nonsmoker and did not consume
alcohol.
On physical examination, healthy-appearing woman, BP 144/66, heart rate 60, respiratory rate 20. Lungs reveals of inspiratory crackles that are fine and without course crackles. There is no lower extremity edema and reveal no finger clubbing.
PFT's: TLC 57% with a DLCO of 50% predicted.
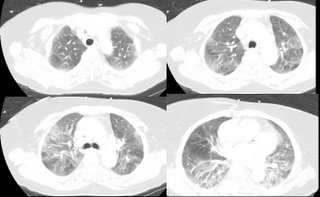
CXR and CT's here:

There was no lymphadeopathy.
Dobutamine echo: no wall motion abnormalities. EF 55-60%. BNP when she came in with SOB was 24. There was no improvement with diuresis.
Transbronchial biopsy: peribronchial tissue with single poorly-formed granuloma. Lung parenchyma with focal type II pneumocyte hyperplasia.
What are your thoughts?
3 comments - CLICK HERE to read & add your own!:
There is a moderately severe restrictive ventilatory defect and impaired gas exchange. The CXR shows a diffuse bilater reticulonodular pattern with some areas of focal increased opacity.
The CT scan shows diffuse, patchy, bilateral, upper and lower lobe ground glass opacities. There are no soft-tissue windows included, so I'm not sure about lymph nodes. There do seem to be some abnormalities in the pre-vascular, A-P window, and pre-tracheal regions; so if these are nodes, they are calcified.
In the differential, I would consider BOOP/COP, idiopathic interstitial pneumonias (not typical for IPF, lack of smoking history makes DIP/RBILD unlikely, AIP is possible, especially in light of the acuity, but rare, and NSIP remains a possibility although the onset would be rapid).
I agree that we need to consider granulomatous disease: the distribution is not typical for sarcoid or HP, althoug acute HP could have this presentation. Endemic fungi and TB are also in the realm of possibility.
Other bacterial infections are possible, but would not explain the restriction.
Malignancy- BAC in particular, could look like this, but again, the acuity would be very atypical.
My best guess(es) at this point: 1) BOOP, 2) Acute HP, 3) Infection
Regardless, I would proceed with bronchoscopy (with BAL and TBBx primarily to evaluate for infection), and then a surgical lung biopsy.
Agree with JCH's differential.
I would move HP to the top of my list given the acuity, the lack of a lobar infiltrate and the fine rales.
BOOP should give a more lobar infiltrate.
Can you give more history on any exposures, funky pets, or work/home environment?
Other studies I would get would be:
ESR, CRP, RF, ANA, hypersenstivity pneumonitis panel and bilateral knee films.
Unless something jumps out at you on these studies, I would get a SLB.
The patient does not speak English so the history is from the daughter; nonethess, no exposure history could be ascertained; no birds. No unusual hobbies. No occupation. There is no known TB exposures.
I agree that the most likely diagnoses are HP (despite success in obtaining a positive exposure history) and COP (previously known as idiopathic BOOP).
The single poorly-formed granuloma seen on tbbx is interesting but I think an open lung will be needed...
Post a Commenttest post a comment