3-4 weeks ago, became progressively more dyspneic. Initially noted with moderate amts of exertion, but now is at rest. Denies any cough, sputum. Has some pleuritic CP. Still having intermittent fevers, chills and sweats.
No TB risk factors.
PMH: Hypertension, hyperlipidemia
FH: nothing strange (i.e. only HTN, DM2, CAD, etc)
No new meds. He is on a statin, (LFT’s have been stable since placement on this drug 9 months ago), BBlocker, aleve
PE: Temp 38.4; 90% on RA at rest… desaturates to 85% with 4 minutes of walking
Lungs: Clear
Tatoos on both upper extremities (professionally done)
Basic labs normal except AST and ALT in 400’s. They have not appreciably changed in 6 months.
Hepatitis panels negative; Abd u/s shows some “fatter liver” with boarderline splenomegaly
PFT’s

The CXR showed interstitial pattern; to save space, I will not include it. Most would have gotten a CT in f/u anyway.
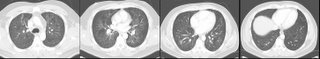
CT (not high resolution)
What would you do next?
6 comments - CLICK HERE to read & add your own!:
First, I would make sure he doesn't have heart failure, as this would be a compatable dx with the history of DOE, restrictive PFT's and ground glass opacities on CT.
After that I would do a bronch to rule out infection. This is less likely with the chronic course I realize. I wuld then send a cell count to look for 1. eosinophils, 2. lymphocytes (for the HP vs sarcoid route as Doung touched on). Then I would send off a TBBx to see if there are any surprises (like a noncaseating granuloma). After that if there is still no diagnosis I would send for surgical biopsy to look for HP or perhaps RSB-ILD or DIP (does he smoke?).
I am also having trouble reconciling the LFT abnormalities with the lung changes. HCV with mixed cryoglobulins and pulmonary-vascular abnormalities could be a start but ML listed a negative hep panel. Likewise, HIV may explain the breadth of systems involved... what was the HIV status?
I like the HP possibility and it may account for some of the constitutional symptoms. Disseminated chronic histoplasmosis may cause direct liver involvement (and not be picked up on the viral Hep panel) and pulmonary infiltrates. Histo Ag and bronch would help.
TB can certainly look odd on presentation even with no obvious exposure.
Spirochetes like Doug suggested can involve lungs and liver but their course tend to be more acute...
Sarcoid was also mentioned. It can have some systemic symptoms and involve the liver (though that's fairly uncommon).
Vasculitides can also affect multiple systems and present with constitutional symptoms though I am having trouble joining the liver and lungs: PAN usually involves the liver but rarely the lungs, Wegener's and microscopic poliangiitis don't cause as much liver disease...
I was much more confused than all of you. I did, however, send an HIV test from the office on a hunch similar to Doug's.
I bronched him the next day and the cytopathologist called me with (+) PCP in the BAL.
The HIV test came back later that day as positive as well.
ID thinks he has an "HIV Hepatopathy." I am unsure what this means.
Anyway, with bactrim IV he rapidly improved and was d/c from the hospital in 3 days.
What was his CD4 count? If he is <50, disseminated MAI may explain the liver abnormalities and constitutional symptoms as well.
Cannot read the pft's results. Is there a way to get them bigger or sharper image?
I would say that he has the rare interstitial lung disease LAM or lymphangioleiomyomatosis from the symptoms CT and PFT.
Post a Commenttest post a comment