This is an outside submission for a question correlating a pleural effusion and Gyn disease:
Patient with a right pleural effusion, more than 1500 ml tapped. 2nd tap: more than 1700 ml tapped 6 days later. Contrast CT revealed pelvic fibroids.
Effusion results protein, probably assoc. w/ RBC.5 to 11 months prior, sonograms, contrast MRI revealed uterine fibroids 8 to 10 mm in size, stable in size over 6 months. Uterine scrape (not complete D and C) test benign. No indications of ovarian cysts, etc. Hysterectomy not chosen due to stable fibroid size and results of uterine scrape.Heavy coughing for 9 mos. Chronic post-nasal drip for 23 mos.
Allergy tests reveal slight allergy to a few local plants.
Chest xray showed: Pleural effusion right side.
Latest contrast CT pelvic fibroid.Previous ultrasound and contract MRI showed uterine fibroids stable after approx 6 mos.
Effusion samples from 2 taps have no cytology assoc. w/cancer, no pancreatitis, tb/fungus results not yet available. Unremarkable except for protein.
2D echo unremarkable.
Any suggestions on this reaccumulating effusion?
Thursday, August 31, 2006
Wednesday, August 30, 2006
Diagnosis and staging of lung cancer
Anonymous asks, If a patient, on chest CT, has a mass invading the hilum and mediastinum and there is also a pleural effusion, would you be able to simply do a thoracentesis for cytology and forego the bronch?
My take is that a bronchoscopy would not be neccessary, as a positive effusion will both diagnose and stage it as a T4. What do you think?
My take is that a bronchoscopy would not be neccessary, as a positive effusion will both diagnose and stage it as a T4. What do you think?
Monday, August 28, 2006
35 year old with cough, chills
35 year old without PMhx except a MVA 5 years ago, anxiety and depression. Now with chills and subjective fever and weight loss for the past few months. Meds: Paxil. Fhx: brother died of liver failure, patient does not know etiology. SH denies IVDA. 2 PPD x 20 years. Quit 5 yrs ago. HIV negative. Exam Afebrile. VSS. Some decr breath sounds upper lung zones b/l. WBC 11.

What would you do next?

What would you do next?
Alpha-1 AT
So, I saw a patient last week for Alpha-1 AT deficiency. Phenotypically, she has the disease--lower lobe emphysema, severe obstructive disease (FEV1 of 1.0 L which improved to 1.35 while on augmentation therapy with Prolastin). She has a family history of the disease and is a non-smoker (with substantial second-hand exposure). Her measured enzyme level, prior to the start of weekly Prolastin, was 31 mg/dl (lab range for normal is 100-190 mg/dl).
So, the interesting thing is that she (and her family members with the disease) has an M-Z genotype, which should be a "normal" phenotype without disease. The genotype was confirmed with separate studies, as was her son's genotype.
Anyone seen this before? Any comments?
So, the interesting thing is that she (and her family members with the disease) has an M-Z genotype, which should be a "normal" phenotype without disease. The genotype was confirmed with separate studies, as was her son's genotype.
Anyone seen this before? Any comments?
Thursday, August 24, 2006
Prune-belly
I have just seen a 26 y/o patient in the office for recurrent respiratory tract infections. He has a Hx of prune-belly syndrome (poor abdominal muscle development with severe urinary tract abnormalities) and has been on HD after a failed renal Txp.
These patients tend to have a restrictive physiology because of the oligohydramnios and sometimes even have hypoplastic lung. Indeed his TLC is ~66%. His Cxr is pretty unremarkable but he also has an associated obstructive defect: FEV1 is ~36% witha ratio of<70%. Has anybody seen this condition (or similar ones) be associated with asthma/reactive airways disease?
These patients tend to have a restrictive physiology because of the oligohydramnios and sometimes even have hypoplastic lung. Indeed his TLC is ~66%. His Cxr is pretty unremarkable but he also has an associated obstructive defect: FEV1 is ~36% witha ratio of<70%. Has anybody seen this condition (or similar ones) be associated with asthma/reactive airways disease?
Tuesday, August 22, 2006
CPET
What do you think of this CPET data?
61 y/o obese woman (BMI: 37.3), S/P remote CABG with patent grafts and normal LVEF on recent angiography with persistent DOE. Very remote smoking Hx with only a mild restrictive defect (FVC~70% with FEV1/FVC>80), normal DLCO and normal HRCT. Negative methacholine challenge.
DATA (predicted values and/or percentages):
VO2max (ml/kg/min): 14.4 (25.4/56%)
AT: 0.749 (>0.698) - 43% predicted VO2max (>40%)
Max HR 73% predicted with still good reserve: 44. O2 pulse 11.5 (8.4)
VE max: 50.7 (65.9 / 77%)
Vt: 1.28 (0.563)
Respiratory rate: 36 (<50)
Breathing reserve: 2% (20-40%)
Vd/Vt at rest: 0.51 (0.30)
Vd/Vt at peak: 0.26 (0.18)
RQ: 0.93 (1.1-1.3)
No desat.
FVC at peak declined by 19% and FEV1 at peak did not change.
61 y/o obese woman (BMI: 37.3), S/P remote CABG with patent grafts and normal LVEF on recent angiography with persistent DOE. Very remote smoking Hx with only a mild restrictive defect (FVC~70% with FEV1/FVC>80), normal DLCO and normal HRCT. Negative methacholine challenge.
DATA (predicted values and/or percentages):
VO2max (ml/kg/min): 14.4 (25.4/56%)
AT: 0.749 (>0.698) - 43% predicted VO2max (>40%)
Max HR 73% predicted with still good reserve: 44. O2 pulse 11.5 (8.4)
VE max: 50.7 (65.9 / 77%)
Vt: 1.28 (0.563)
Respiratory rate: 36 (<50)
Breathing reserve: 2% (20-40%)
Vd/Vt at rest: 0.51 (0.30)
Vd/Vt at peak: 0.26 (0.18)
RQ: 0.93 (1.1-1.3)
No desat.
FVC at peak declined by 19% and FEV1 at peak did not change.
Monday, August 21, 2006
Anemia
This is more of a critical care than pulmonary question. It came up today in discussion with renal...
The gold satndard for iron-def. anemia has been staining the bone marrow for iron stores. Nobody does that much anymore as first test since ferritin has such a good correlation with iron stores. The discussion was whether you can have iron-deficiency anemia with good normal ferritin (not normal-low, low-normal, borderline, etc.). Even though ferritin is an acute phase reactant and may mak a borderline ferritin level seem normal it shouldn't push it to the mid-high range. (ferritin will roughly triple as an acute phase marker, Ann Rheum Dis 1986 Jul;45(7):596-602)
Do you look at the iron/iron sat or do you trust the ferritin?
The gold satndard for iron-def. anemia has been staining the bone marrow for iron stores. Nobody does that much anymore as first test since ferritin has such a good correlation with iron stores. The discussion was whether you can have iron-deficiency anemia with good normal ferritin (not normal-low, low-normal, borderline, etc.). Even though ferritin is an acute phase reactant and may mak a borderline ferritin level seem normal it shouldn't push it to the mid-high range. (ferritin will roughly triple as an acute phase marker, Ann Rheum Dis 1986 Jul;45(7):596-602)
Do you look at the iron/iron sat or do you trust the ferritin?
Thursday, August 17, 2006
Failure to wean
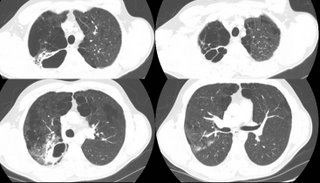
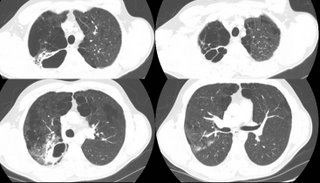
This is a 44 year old man with DM, s/p renal transplant several years ago. He has the other associated micro- and macro- vascular problems associated with DM, including severe PVOD and a non-healing, chronic LE cellulitis for which a BKA has been recommended (but refused--he is on chronic supressive antibiotics). His immunosupression includes cyclosporine and prednisone.
He was admitted to the ICU with hypoxemic respiratory failure requiring intubation for what turned out to be herpes pneumonitis, and was treated with a 21 day course of acyclovir. Over this course, he was easily ventilated and oxygenated with progressively improving respiratory parameters. On two occasions, his weaning parameters were excellent, and he easily tolerated minimal ventilatory support (PS-5/PEEP 5) for 2 hours. Each time, he required re-intubation for respiratory distress several hours after extubation.
Here's some representative cuts from a CT scan done about 10 days into his hospital course.

He was admitted to the ICU with hypoxemic respiratory failure requiring intubation for what turned out to be herpes pneumonitis, and was treated with a 21 day course of acyclovir. Over this course, he was easily ventilated and oxygenated with progressively improving respiratory parameters. On two occasions, his weaning parameters were excellent, and he easily tolerated minimal ventilatory support (PS-5/PEEP 5) for 2 hours. Each time, he required re-intubation for respiratory distress several hours after extubation.
Here's some representative cuts from a CT scan done about 10 days into his hospital course.

Tuesday, August 15, 2006
PET and staging
I saw this patient in follow-up today.
This is an 82 y/o woman with no smoking history but decades of second-hand smoke (her husband died of lung dz). She had a dry cough and a CT scan was done. She has the large LUL mass seen on the CT cut (on an outside CT with contrast, the mass seems to invade the PA). I did a bronch and the mass is a non-small cell Ca. Unfortunately, the hilar TBNA were non-diagnostic. Her PET scan shows marked uptake by the mas, ipsi- and contralateral hilar nodes and pre-tracheal nodes.
With the PA involvement (on CT) and the PET results would you be satisfied in calling it a IIIB or would you do a mediastinoscopy to confirm either/both with tissue?

This is an 82 y/o woman with no smoking history but decades of second-hand smoke (her husband died of lung dz). She had a dry cough and a CT scan was done. She has the large LUL mass seen on the CT cut (on an outside CT with contrast, the mass seems to invade the PA). I did a bronch and the mass is a non-small cell Ca. Unfortunately, the hilar TBNA were non-diagnostic. Her PET scan shows marked uptake by the mas, ipsi- and contralateral hilar nodes and pre-tracheal nodes.
With the PA involvement (on CT) and the PET results would you be satisfied in calling it a IIIB or would you do a mediastinoscopy to confirm either/both with tissue?

Monday, August 14, 2006
Outside case: Adenopathy
This was submitted to us:
34yr.old female w/ previous rt low lobe nodules since 2001 CT revealed the nodules while patient had chickenpox.
New CT in 2006 shows new node on lt. upper diaphragm. Last CT 6mo. prior didnt show nodule, which is uncalcified unlike rt. lung nodes.
PT. has nightsweats wt. loss chronic pelvic abdominal pain jointpain/swell/stiff no appetite ab.bloat chronic urinary symptoms and UTI.
Now with SWOLLENLYMPHNODES W/LYMPH SURFACING AND RUPTURE ON NECK BACK OF HEAD BEHIND EAR. PT. is 11/2 ppd smoker of 13yrs. PET done 4/06 and no malignant chest activity. labs almost normal.
34yr.old female w/ previous rt low lobe nodules since 2001 CT revealed the nodules while patient had chickenpox.
New CT in 2006 shows new node on lt. upper diaphragm. Last CT 6mo. prior didnt show nodule, which is uncalcified unlike rt. lung nodes.
PT. has nightsweats wt. loss chronic pelvic abdominal pain jointpain/swell/stiff no appetite ab.bloat chronic urinary symptoms and UTI.
Now with SWOLLENLYMPHNODES W/LYMPH SURFACING AND RUPTURE ON NECK BACK OF HEAD BEHIND EAR. PT. is 11/2 ppd smoker of 13yrs. PET done 4/06 and no malignant chest activity. labs almost normal.
Wedding bells
Congratulations to one of our editors: Jeff Jennings tied the knot this past weekend.
We will keep posting while he is on his honeymoon.
We will keep posting while he is on his honeymoon.
Wednesday, August 09, 2006
Acid Base
The chem-7 and the gas were both drawn within 22 minutes of each other in this 71 year old intubated man with sepsis and ARDS:
7.08/24/226 on fio2 of 75%
Na 145
k 5.2
Cl- 114
HCO3 28
BUN 42
Cr 0.5
What is the acid base disturbance?
7.08/24/226 on fio2 of 75%
Na 145
k 5.2
Cl- 114
HCO3 28
BUN 42
Cr 0.5
What is the acid base disturbance?
Proceed or watch? Is it CA?
Here is a case submitted to us:
8/1/06 49 YO Caucasion male, married with minor children, comfortably employed professional, USAF Gulf War Veteran, 2-3 PPD smoker X30 years, ETOH dependent (averages 6-10 beers daily)presents with R clavicular pain after home remodeling project. Well developed, well nourished, muscular, athletic body type. VS WNL. Non remarkable EKG. Clavicle XR demonstrates shoulder separation with incidental 1.75cm diameter spiculated nodule mid upper right lobe lung, mild emphysematous changes. CT confirms nodule. PET eyes to knees results no demonstrative uptakes. CBC, Metabolic panels normal. CEA and CA125 WNL. PFTs near normal, demonstrates ability to tolerate surgery.
Family HX: Maternal died d/t +NSCL CA with brain, liver mets. Paternal +adenocarcinoma colon, in remission post colectomy and chemo. No other significant family HX or disease.
Smoking Cessation in process with nicotine patch use. ETOH use diminishing. Pt. wants no invasive surgery or BX unless absolutely indicated. Lesion is not near bronch, no bronchoscopy in plan. What next?
8/1/06 49 YO Caucasion male, married with minor children, comfortably employed professional, USAF Gulf War Veteran, 2-3 PPD smoker X30 years, ETOH dependent (averages 6-10 beers daily)presents with R clavicular pain after home remodeling project. Well developed, well nourished, muscular, athletic body type. VS WNL. Non remarkable EKG. Clavicle XR demonstrates shoulder separation with incidental 1.75cm diameter spiculated nodule mid upper right lobe lung, mild emphysematous changes. CT confirms nodule. PET eyes to knees results no demonstrative uptakes. CBC, Metabolic panels normal. CEA and CA125 WNL. PFTs near normal, demonstrates ability to tolerate surgery.
Family HX: Maternal died d/t +NSCL CA with brain, liver mets. Paternal +adenocarcinoma colon, in remission post colectomy and chemo. No other significant family HX or disease.
Smoking Cessation in process with nicotine patch use. ETOH use diminishing. Pt. wants no invasive surgery or BX unless absolutely indicated. Lesion is not near bronch, no bronchoscopy in plan. What next?
Tuesday, August 08, 2006
Mass and infiltrates
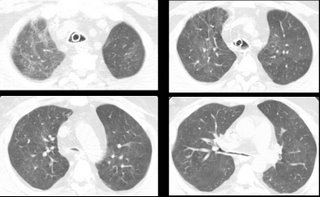
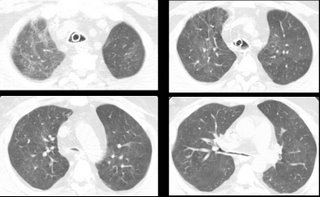
This is a 59 y/o woman with a funny presentation: she had an episode of syncope at home, hit her head and had a skin lac requiring 7 stitches. While being worked up in the ER they found her to be hypotensive and febrile with an abnormal CxR and CT of the chest. She had MSSA in her sputum and the dense "mass" seen on the left images. I bronch'ed her and got "organizing pneumonia" but no malignancy. She got ABTx and the "mass" went away completely.
She has felt better and has good PFTs. However, it has now been 3 months and the peripheral faint patchy areas of reticular disease remain there and unchanged.
She has only minimal DOE. She quit smoking in 1988 and has no unusual exposures.
How would you pursue this little infiltrates? (they are present in the lower lobes as well).

She has felt better and has good PFTs. However, it has now been 3 months and the peripheral faint patchy areas of reticular disease remain there and unchanged.
She has only minimal DOE. She quit smoking in 1988 and has no unusual exposures.
How would you pursue this little infiltrates? (they are present in the lower lobes as well).

Thursday, August 03, 2006
Halleliujah
From Arenberg:
"In celebration of the fact that the IT people in the Department of Radiology at the University of of Michigan have recognozed that their department exists to provide films for other doctors to look at, and have finally made it into the 21st centry by providing consistent, relaible online access to films for the unwashed masses (read: non-radiologists)...I hereby submit this film of an unfortunate man with a history of cancer."

"In celebration of the fact that the IT people in the Department of Radiology at the University of of Michigan have recognozed that their department exists to provide films for other doctors to look at, and have finally made it into the 21st centry by providing consistent, relaible online access to films for the unwashed masses (read: non-radiologists)...I hereby submit this film of an unfortunate man with a history of cancer."

Subscribe to:
Posts (Atom)