This woman had presented with hemoptysis once and a CT scan showed tree in bud pattern and some nodularity. She presented a year later with cough and sputum. A culture had previously shown 1/3 AFB + but non-TB and non-avium. Her symptoms are the daily cough without constitutional symptoms and no shortness of breath.
I sent off a sputum and it showed Many PMNs, few Epithelial cells, many Gram positive cocci in pairs, chains and clusters and rare Gram negative bacilli.
What would you do now?
Monday, October 30, 2006
The Philosophy of Disclosure
From AK:
I'm sure most of us have seen some close variation on this clinical theme: a smoker has a suspicious lung mass with evidence of metastasis elsewhere, and you're consulted to help get tissue. The patient hasn't seen the scans, doesn't know the overwhelming odds that they have metastatic lung cancer. As a consultant, how much should you tell the patient before you have path results? If they ask about the possibility of surgical resection, is it right to put off an answer you know is highly likely to be correct?
I'm sure most of us have seen some close variation on this clinical theme: a smoker has a suspicious lung mass with evidence of metastasis elsewhere, and you're consulted to help get tissue. The patient hasn't seen the scans, doesn't know the overwhelming odds that they have metastatic lung cancer. As a consultant, how much should you tell the patient before you have path results? If they ask about the possibility of surgical resection, is it right to put off an answer you know is highly likely to be correct?
Thursday, October 26, 2006
Lung cancer screening
The International Early Lung Cancer Action Program Investigators published the results from CT screening >30,000 patients with chest CTs in today's NEJM.
They found a shift towards picking up more early stage disease.
Have you had a chance to see the study? How do you think this will affect our practice?
They found a shift towards picking up more early stage disease.
Have you had a chance to see the study? How do you think this will affect our practice?
Wednesday, October 25, 2006
Treatment of GERD
How do you make a determination to treat for GER in patients with asthma?
There is some data available saying that treatment may reduce exacerbations and improve quality of life...
Littner MR, Leung FW, Ballard ED 2nd, Huang B, Samra NK; Lansoprazole Asthma Study Group.
Effects of 24 weeks of lansoprazole therapy on asthma symptoms, exacerbations, quality of life, and pulmonary function in adult asthmatic patients with acid reflux symptoms.
Chest. 2005 Sep;128(3):1128-35.
PMID: 16162697 [PubMed - indexed for MEDLINE]
There is some data available saying that treatment may reduce exacerbations and improve quality of life...
Littner MR, Leung FW, Ballard ED 2nd, Huang B, Samra NK; Lansoprazole Asthma Study Group.
Effects of 24 weeks of lansoprazole therapy on asthma symptoms, exacerbations, quality of life, and pulmonary function in adult asthmatic patients with acid reflux symptoms.
Chest. 2005 Sep;128(3):1128-35.
PMID: 16162697 [PubMed - indexed for MEDLINE]
Preop eval for secondary HTN due to severe COPD
Redneck pulmonologist submits this question:
Would you do anything for secondary pulmonary hypertension (estimated PAP of 80-90 mmHG on echo) due to COPD before undergoing renal transplant? Her COPD is 2 to AAT deficiency and stable on AAT replacement. FEV1 of 40% predicted. She has documented nocturnal desat on sleep study without significant sleep apnea. But she is non-compliant with home O2. Daytime sat on RA is OK. She is not a smoker. She is on dialysis and her ESRD is due to pauci-immune vasculitis and has been treated with steroids and Cellcept. Work up for other causes of secondary pulmonary HTN is negative.
Would you do anything for secondary pulmonary hypertension (estimated PAP of 80-90 mmHG on echo) due to COPD before undergoing renal transplant? Her COPD is 2 to AAT deficiency and stable on AAT replacement. FEV1 of 40% predicted. She has documented nocturnal desat on sleep study without significant sleep apnea. But she is non-compliant with home O2. Daytime sat on RA is OK. She is not a smoker. She is on dialysis and her ESRD is due to pauci-immune vasculitis and has been treated with steroids and Cellcept. Work up for other causes of secondary pulmonary HTN is negative.
Tuesday, October 24, 2006
Is this BOOP, Y-J?
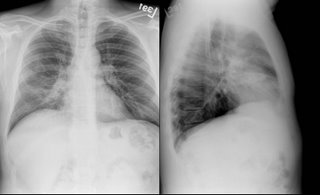
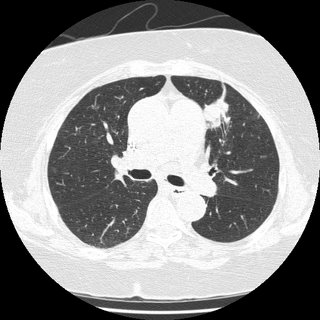
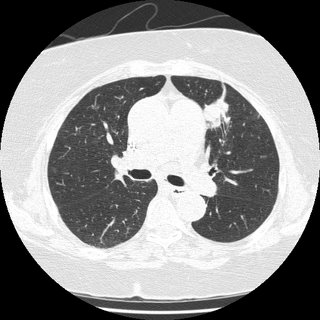
41 yo male who works for a satellite dish installation company presented with progressive dyspnea over a couple of months. An urgent care CXR was (+) for a nodule in the R mid lung field, and he was referred to his PCP; he received no intervention at that time. He was lost to f/u and ultimately presented with progressive symptoms one month later. His PCP obtained a CT (see below) and he was sent to be admitted. Upon seeing him, he look chronically ill, but not toxic.

I bronched him, and it was non-diagnostic. I sent him for a surgical biopsy.
The report was read as BOOP with an microscopic sulfur granules c/w actinomycosis.
I started him on Augmentin and saw in the office in 3 weeks.
He was no better. Spiro was c/w were moderate restrictive vent defect.
So, I started him on steroids at 40 mg/day of prednisone x 3 weeks then 30 mg/day.
I saw him 4 weeks later (about 1 week into his 30 mg/day) without any clinical improvement.
His full PFT's are c/w mild obstruction with air trapping and impaired gas exchange (DL ~70% predicted). He is a smoker, and is still smoking about 1/2 ppd.
I had his biopsy reviewed by Jeff Myers at U of M (profoundly smart and helpful- wish he would have joined the faculty 5 years sooner), but he thought the original interp was correct.
Now what?

I bronched him, and it was non-diagnostic. I sent him for a surgical biopsy.
The report was read as BOOP with an microscopic sulfur granules c/w actinomycosis.
I started him on Augmentin and saw in the office in 3 weeks.
He was no better. Spiro was c/w were moderate restrictive vent defect.
So, I started him on steroids at 40 mg/day of prednisone x 3 weeks then 30 mg/day.
I saw him 4 weeks later (about 1 week into his 30 mg/day) without any clinical improvement.
His full PFT's are c/w mild obstruction with air trapping and impaired gas exchange (DL ~70% predicted). He is a smoker, and is still smoking about 1/2 ppd.
I had his biopsy reviewed by Jeff Myers at U of M (profoundly smart and helpful- wish he would have joined the faculty 5 years sooner), but he thought the original interp was correct.
Now what?
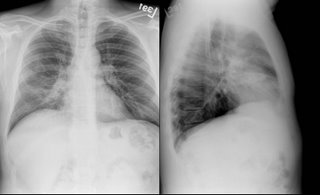
tree in bud in a 66 year old.
66-year-old lady who presented initially to our Pulmonary Clinic 2 years ago for evaluation of a one-time episode of hemoptysis. A CT of her chest showed focal areas of local bronchiectasis, tree-in-bud pattern. There was a concern about atypical mycobacteria and sputum cultures were obtained. Only one of those was positive for
non tuberculous mycobacteria. Since she was asymptomatic she was merely followed. A year later she has a bit of a nagging cough but no constitutional symptoms. However, a follow-up chest CT showed decrease in the nodularity in the outer lower
aspect of the right upper lobe, but increased atelectasis
and thickening around several bronchi the areas in the medial segment
of the right middle lobe.
In terms of management, how would you proceed, given the slight worsenening radiographically?
non tuberculous mycobacteria. Since she was asymptomatic she was merely followed. A year later she has a bit of a nagging cough but no constitutional symptoms. However, a follow-up chest CT showed decrease in the nodularity in the outer lower
aspect of the right upper lobe, but increased atelectasis
and thickening around several bronchi the areas in the medial segment
of the right middle lobe.
In terms of management, how would you proceed, given the slight worsenening radiographically?
Friday, October 20, 2006
Follow-up to "What is wrong with this picture?"
I thought this was pretty interesting CT scan...
This patient has congenital atresia of the R pulmonary artery with absent R pulmonary circulation (this was a CT-A so you can see some opacified vessels on the L but none on the R). He likely only has some systemic (bronchial) circulation on the R. He has no pulm HTN on ECHO (no surprise, people do survive pneumonectomies) but we counselled him strongly on smoking cessation...
This patient has congenital atresia of the R pulmonary artery with absent R pulmonary circulation (this was a CT-A so you can see some opacified vessels on the L but none on the R). He likely only has some systemic (bronchial) circulation on the R. He has no pulm HTN on ECHO (no surprise, people do survive pneumonectomies) but we counselled him strongly on smoking cessation...
Wednesday, October 18, 2006
Diagnosis and management questions
Get some feedback from others: Submit a case! If there are too many details (i.e. time consuming), feel free to submit a brief one and people can ask for clarifications in the comments.
Tuesday, October 17, 2006
Abnormal CxR
I usually don't like those boards-type question that ask "what would you do next?" and only let you choose one option since we often do more than one thing in real life.
Having said that, I am curious as to what you would do next in this case. This is kind of a VIP patient so she was referred to a couple different specialists at the same time.
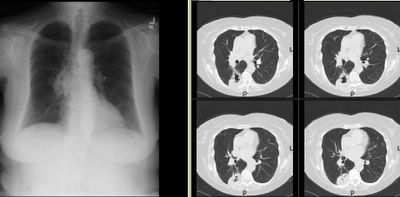
She is in her early 70s, quit smoking in 1972, near normal PFTs (FEV1~70%, normal DLCO) and has an abnormal CxR. It started as an URI and then she developed a "deeper" cough with purulent sputum production and some pleuritic CP.
The abnormal CxR (and some CT cuts) are shown below.
She had no adenopathy on the CT.
What would be your first step?
Having said that, I am curious as to what you would do next in this case. This is kind of a VIP patient so she was referred to a couple different specialists at the same time.
She is in her early 70s, quit smoking in 1972, near normal PFTs (FEV1~70%, normal DLCO) and has an abnormal CxR. It started as an URI and then she developed a "deeper" cough with purulent sputum production and some pleuritic CP.
The abnormal CxR (and some CT cuts) are shown below.
She had no adenopathy on the CT.
What would be your first step?
Monday, October 16, 2006
Shortness of breath
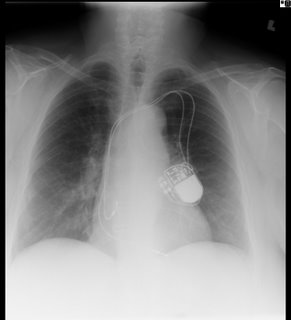
79-year-old man who underwent a four-vessel CABG in January 2006. A few months prior to that, he had developed some malaise and ultimately chest pain leading to an angiogram that revealed 95%, 90%, 80%, and 60% occlusion. After the 4-vessel CABG, he reports shortness of breath worse in the supine position that occurs quite quickly after lying down, perhaps after a minute.
He is able to walk a few miles without significant shortness of breath. He is also able to walk up a flight of stairs with only moderate shortness of breath, and he denies any muscle weakness or achiness. He is able to stand from the sitting position in the chair with a bit of shortness of breath, but no frank weakness. The patient denies any fevers, chills, or night sweats. Furthermore, he denies a cough. There is no productive cough except for the occasional cold about once a year. Rest of his complete review of systems is noncontributory.
On exam it is unremarkable with good air entry bilaterally. In the supine position there is bilateral paradoxical abdominal movement with inspiration.
A CXR is here:
I obtained spirometry in the supine position and repeated that in the upright:
FVC Upright: 2.61L (64% predicted)
Supine: 1.18L (29% predicted) -55% change in vital capacity
PI max cmH2O (51%) 100
PE max cmH2O (104%) 187
It appears he has bilateral diaphragmatic paralysis. It coincides with the CABG, but I think this would be fairly atypical, as that is usually associated with unilateral. In terms of muscle weakness, the low PI but normal PE max argues against this.
Thoughts?
He is able to walk a few miles without significant shortness of breath. He is also able to walk up a flight of stairs with only moderate shortness of breath, and he denies any muscle weakness or achiness. He is able to stand from the sitting position in the chair with a bit of shortness of breath, but no frank weakness. The patient denies any fevers, chills, or night sweats. Furthermore, he denies a cough. There is no productive cough except for the occasional cold about once a year. Rest of his complete review of systems is noncontributory.
On exam it is unremarkable with good air entry bilaterally. In the supine position there is bilateral paradoxical abdominal movement with inspiration.
A CXR is here:
I obtained spirometry in the supine position and repeated that in the upright:
FVC Upright: 2.61L (64% predicted)
Supine: 1.18L (29% predicted) -55% change in vital capacity
PI max cmH2O (51%) 100
PE max cmH2O (104%) 187
It appears he has bilateral diaphragmatic paralysis. It coincides with the CABG, but I think this would be fairly atypical, as that is usually associated with unilateral. In terms of muscle weakness, the low PI but normal PE max argues against this.
Thoughts?
Wednesday, October 11, 2006
Follow up to change in mental status
This patient presented with change in MS. The CXR had shown some patchy markings but nothing specific. But the right hilar was full-looking so a CT was done:

Lung windows:

Thoughts?

Lung windows:

Thoughts?
Tuesday, October 10, 2006
Persistent pleural effusion
This is a 38 year old man who is 1.5 years s/p a bone marrow transplant for non-Hodgekin's Lymphoma that had relapsed despite several chemotherapeutic regimens. His post-transplant course has been generally uneventful, with good engraftment, no major infectious complications, and minimal GVHD of the skin and gut. He also had a DVT at some point, treated with adequate anticoagulation for 9 months. He was referred for a right pleural effusion. This was tapped-it was a chylothorax. Flow-cytometry was negative for a recurrence of the lymphoma.
His pulmonary function varies a bit between normal and a mild obstructive ventilatory defect. His exercise capacity has continued to improve since the BMT, but remains significantly below his pre-morbid state (he was, prior to his cancer, a highly trained endurance athlete).
He is referred for pleuradesis.
His films are below:
His pre-BMT film:

One year later, prior to thoracentesis:

One-day following a 2-liter thoracentesis

Thoughts? How would you proceed?
His pulmonary function varies a bit between normal and a mild obstructive ventilatory defect. His exercise capacity has continued to improve since the BMT, but remains significantly below his pre-morbid state (he was, prior to his cancer, a highly trained endurance athlete).
He is referred for pleuradesis.
His films are below:
His pre-BMT film:

One year later, prior to thoracentesis:

One-day following a 2-liter thoracentesis

Thoughts? How would you proceed?
Monday, October 09, 2006
Change in mental status
45 year old man, presented with a persistant cough that did not go away despite 4 different antibiotic course, some kenalog, some anti-allergy meds, and finally a CXR that showed "Right middle lobe pneumonia"
He was admitted for the persistent cough.
ROS no weight loss, SOB, nightsweats. Just the cough (non productive).
SOCIAL HISTORY: married,self-employed painter. He smokes cigars usually five times a week. He averages six to 12 alcohol beverages per week.
On exam the next day he was alert but confused. His vitals were normal as was his saturation on room air. He did not answer questions. He just looked at his wife and smiled. A Na was 129 when before on admission it was 137. The rest of the labs were unremarkable. LP, EEG and head CT were done but negative. By the trime some of that came back he was already becoming more oriented on his own. The next day he was a/o x 3.
Any feedback before I proceed?
He was admitted for the persistent cough.
ROS no weight loss, SOB, nightsweats. Just the cough (non productive).
SOCIAL HISTORY: married,self-employed painter. He smokes cigars usually five times a week. He averages six to 12 alcohol beverages per week.
On exam the next day he was alert but confused. His vitals were normal as was his saturation on room air. He did not answer questions. He just looked at his wife and smiled. A Na was 129 when before on admission it was 137. The rest of the labs were unremarkable. LP, EEG and head CT were done but negative. By the trime some of that came back he was already becoming more oriented on his own. The next day he was a/o x 3.
Any feedback before I proceed?
Wednesday, October 04, 2006
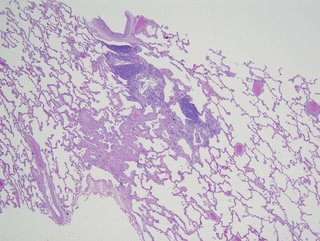
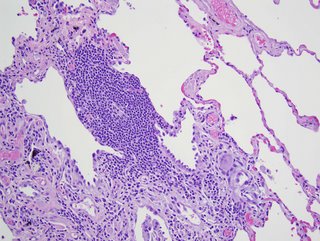
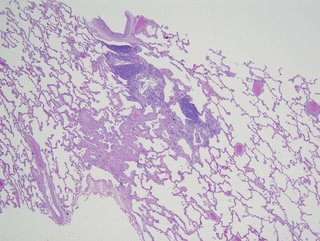
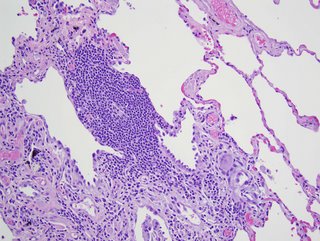
Dyspnea and a LUL mass
Here's a case from Arenberg:
This is 69-year-old lady with coronary artery disease, diastolic congestive heart failure, and dyspnea on exertion. She came to see me because her cardiologist said she has been experiencing increased dyspnea out of proportion to her normal symptoms for ~3 months. Other than a pacemaker over her left chest, her plain chest x-rays were normal
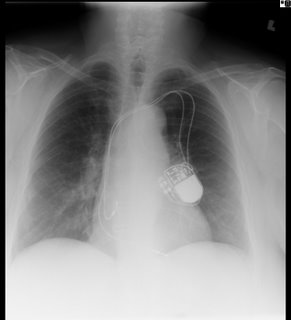
and her pulmonary function tests were mildly restrictive (FVC ~69%), actually improved from her last testing ~ 4 years prior.
I got a VQ scan that was normal, but only on her second visit (when I actually asked) did I learn that she has had 2 birds as house pets for the last 3 years. She further revealed that she has felt unwell going back about 2-1/2 years. One of the birds was in fact sick, and during this time, she fed the bird from mouth to mouth. Yes, I am serious. She was DEAD SET against getting rid of the birds, so I got a CT scan in anticipation of doing a bronch, to prove she had HP.

The CT showed very subtle changes of ground glass, and was actually read as no evidence of ILD, but surprise surprise, she now had a LUL mass that was not seen on the CXR taken 2 months earlier. The radiologist thought it was likely to be inflammatory. What would you do?
I have more images, and some cool pictures to follow, but I’ll hold onto them until people have a chance to comment.
--------------------------
UPDATE:
"...good evidence for chronic HP in the form of a patchy chronic
bronchiolitis that includes occasional multinucleated giant cells of the
sort commonly seen in that condition"
Comments from our pathologist.
This is 69-year-old lady with coronary artery disease, diastolic congestive heart failure, and dyspnea on exertion. She came to see me because her cardiologist said she has been experiencing increased dyspnea out of proportion to her normal symptoms for ~3 months. Other than a pacemaker over her left chest, her plain chest x-rays were normal
and her pulmonary function tests were mildly restrictive (FVC ~69%), actually improved from her last testing ~ 4 years prior.
I got a VQ scan that was normal, but only on her second visit (when I actually asked) did I learn that she has had 2 birds as house pets for the last 3 years. She further revealed that she has felt unwell going back about 2-1/2 years. One of the birds was in fact sick, and during this time, she fed the bird from mouth to mouth. Yes, I am serious. She was DEAD SET against getting rid of the birds, so I got a CT scan in anticipation of doing a bronch, to prove she had HP.

The CT showed very subtle changes of ground glass, and was actually read as no evidence of ILD, but surprise surprise, she now had a LUL mass that was not seen on the CXR taken 2 months earlier. The radiologist thought it was likely to be inflammatory. What would you do?
I have more images, and some cool pictures to follow, but I’ll hold onto them until people have a chance to comment.
--------------------------
UPDATE:
"...good evidence for chronic HP in the form of a patchy chronic
bronchiolitis that includes occasional multinucleated giant cells of the
sort commonly seen in that condition"
Comments from our pathologist.
Tuesday, October 03, 2006
Varenicline
Have you had the chance to start patients on Chantix yet?
What has your experience with it been thus far? Any good success stories?
What has your experience with it been thus far? Any good success stories?
Subscribe to:
Posts (Atom)