Every once in a while we will post questions from patients. Usually we like to keep to the original theme of the blog, which is discussion of cases among health care professinals, but the following case from a patient was interesting. Here it is:I am 23 years old.
I have been diagnosed this past year with heterozygous factor V Leiden.
I have a diagnosis since 12 of asthma, which is treated with Advair 500/50, singulair combivent every 8 hours as needed, albuterol inhaler and nebulizer solution to use every 4-6 hours as needed. I hardly use either.
In January of 2005, I was drinking some hot chocolate and I aspirated on it, which caused an instant response of coughing (obviously), but I started to cough up bright red blood. This turned into a LOT of bright red blood, no sputum. I ended up coughing up about 100mL of blood or more - I never measured it. I was brought to the ER, where I had an x-ray taken, and a laryngoscopy (sp?), I coughed up another 10-15ml of blood while there. I was told that I probably burst a blood vessel in my lung and I was sent home. The next day, I coughed up a long, dark red-black clot of tissue and blood, then I began coughing up blood again, another 15-20mL. It stopped, I did not return to the hospital, as I was told I would continue. The next day, the same thing happened, except less, maybe 10mL of blood.
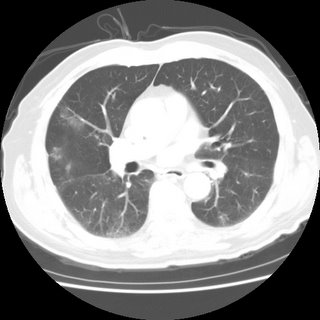
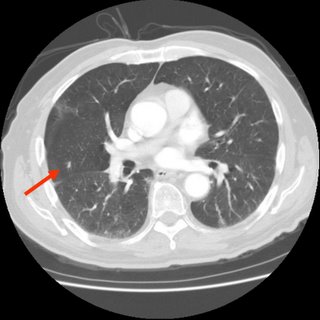
I didn't think anything of it until the next month, toward the end of February while I was shopping with my mother, and I got into the car and suddenly the hemoptysis began again, for no reason. I had not coughed, I just felt a small rumble in my chest and the need to cough the liquid up. Once again, there was bright red blood. My mother took me to the ER, there was less blood this time, and they did a D-dimer, which came back abnormal. In the time I was waiting for the result for the d-Dimer, they did a chest x-ray, which showed nothing significant. Afterward, they did a V/Q scan with both the IV and the nebulizer of the tracer dye. It too was inconclusive. So they sent me to CT to get a scan with dye. That was inconclusive as well. I was admitted to the hospital, and they sent me to get an angiogram. Finally, they found a small clot in my lower left lobe. I was started on heparin, and kept in the hospital for 4-5 days, I don't remember exactly. On the last day, they started me on Lovenox and warfarin, and then they sent me home. This was a friday, I was told to be on bedrest, I also had not moved. The morning after I had been admitted, they had done a doppler ultrasound (duplex) of my legs, and found no clots in my legs. Apparently, there was an "artifact" from the CT or the angio that they saw in my pelvis, but it was a motion artifact, so they didn't see it clearly. Anyway, on Monday, after only four days combined warfarin/Lovenox therapy, my INR was tested, and it was 2.8, so the nurse told me to stop the Lovenox. I did, and the next day I felt pain in my right shoulder blade area that radiated into my ribcage eventually. I called my doctor's office and they told me to call 911. I did, was taken to the ER, my INR was 2.4. Another CT with dye was taken, and this time I had a clot in each lobe of my right lung, along with pulmonary infarct. Each time this happened, my O2 sats were 100 or 99. I was admitted, put back on heparin, and tested for clotting disorders, told I had anticoagulation failure, and had a permanent greenfield filter placed in my inferior vena cava, right above my pelvic veins. I coughed up blood a few days into this one as well. Although I was not told at the time, apparently there was a nodule that was noticed in the CT scan. I will bring this up momentarily.
I decided I didn't trust these doctors, especially after they put me on both warfarin and Lovenox indefinitely. After 7 days of Lovenox at 140mg 2x day S/Q (I weighed 330lbs or so at the time), I began to have "massive hemoptysis" (their words - it was around 100mL - nothing I hadn't done before). This was on March 12, my birthday. I was again in the car, and at the time I had pneumonia, which I had taken home from the hospital with me. I had been on a dose of a z-pak, as well as some other anti-biotic, but I don't recall what it was. Anyway, I went to a different hospital, where they admitted me and again a CT was done with dye, the same clots were seen. They, too, saw the granuloma (calcified) in my lung, the right side, and again, it wasn't mentioned. My anti factor Xa levels were extremely high, so the Lovenox was discontinued. I was hospitalized for 12 days, as my INR stabilized for the FIRST TIME. I coughed up blood a few more times over the next couple of days after the first day I was there, as it seemed I would always do after a first episode, once again coughing up a big clot of blood and then bright red fresh blood before stopping. I would eat cough drops and drink cough syrup.
After my release, I was once again told I would remain on warfarin, basically, for life, due not only to my filter, but to my previous PE and my FVL diagnosis. I didn't cough up anymore blood until my INR was around 2.7, in June, because I was concerned that it tended to hover around 1.8-2.2, and I was afraid of another clot. Then they raised my dose another 2.5mg per week. I was taking a total of 65mg a week. At the end of July, I had another episode of hemoptysis, only around 50ml, I went to the ER, they did a CT scan with dye, told me I had bronchitis, sent me home with antibiotics. Again it happened in August, they listened to my lungs, said I had bronchitis, sent me home, same amount of blood. Again at the end of October, they did an x-ray, sent me home. Each time, it was around the same amount of blood. Each time, there was no coughing prior to it. Nothing to make it seem like I had a cold. My INR was not too high, it was always in range. I was also getting non-injection dye CT scans to follow the granuloma by my pulmonologist, and so far, it has remained stable. It's classified as a "nodule", pretty small, I've had it recently suggested that it may be a harmatoma. Whatever it is, it's half calcified. I did not cough up blood at all during November or December, and for most of January. Then, last Tuesday, I began actually coughing, as I've had a cold since the beginning of November (go figure), and I coughed pretty hard, and immediately began feeling the rumble of blood in my lungs. I begain coughing up bright red blood, rather violently a few times, as though I couldn't quite get it out. My pulmonologist told me that the next time I did this, I was to go to the ER and demand a bronchoscopy, so that's exactly what I did. Except when I got to the ER, they admitted me, I did measure how much I coughed up, it was 100mL of blood. They got me in a room, and scheduled a bronch for the next afternoon, and my INR that evening was 1.7. The next morning it was 1.8. They wanted it closer to 1, so they insisted on giving me FFP, three units, which I turned out to have an allergic reaction to at the last minute of the last bag, or it may have been the vitamin K shot they gave me, either way, my INR was only 1.4 when they checked it again. And I had a shot of 50mg of benedryl. And the bronch was canceled. The pulmonologist on duty wanted to instead do an arterial angiogram to see if I had a harmatoma with bleeding vessels that was causing me to cough up blood and to see if she could embolize them. But the other docs vetoed her, so nothing happened that day. The next day, again a bronch was scheduled, and my INR was still 1.4, but they did the bronch anyway because I refused additional FFP because of the allergic reaction. The bronch showed nothing. The day before I coughed up an additional 50mL of blood. They decided to take me off the warfarin, saying it was too dangerous for me to be on it. They think it is the warfarin causing me to cough up blood all the time.
I have many questions, some of them may be able to be answered by pulmonologists, some of them not.
Is it more likely that I have a harmatoma or a granuloma?
Is it likely that the nodule is the cause of my hemoptysis or the warfarin?
Could an INR of 1.7 cause me to cough up /that/ much blood?
Could being off of warfarin for a month put me at increased risk of pulmonary embolism?
Is all this hemoptysis ruining my lungs?
What is wrong with my lungs?
I know that without actually seeing me, reviewing my records in depth, seeing my scans, x-rays, etc, it's very hard to know the answers, I just want to know what other people think, since I've been seeing the same doctors for a year now, and nobody knows what the heck is wrong with me. I'm at my wits' end. And I'm terrified.