Friday, December 30, 2005
Happy New Year!
Happy new year from the editors of Pulmonary Roundtable. Please come back and visit us again in 2006.
Thursday, December 29, 2005
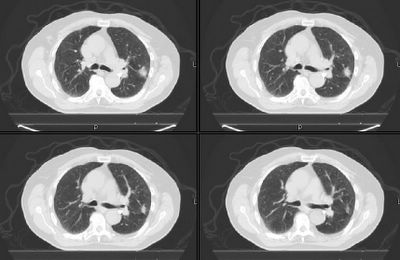
Another 80 year old with a lung lesion.
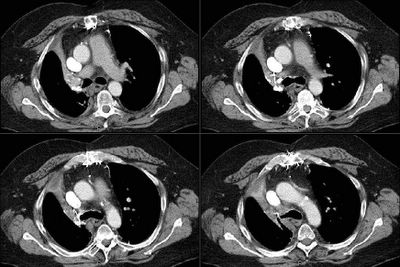
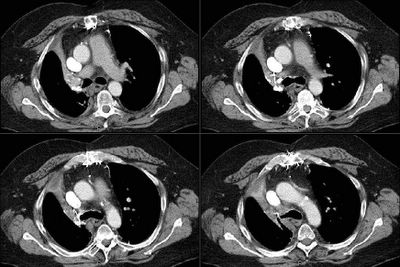
Remember this post about the 80-ish year old with a solitary lesion and whether his age should preclude w/u for possible resection? Well, what would you do with this 82 year old with a hilar (i.e. unresectable) mass that is (as of yet) without diagnosis (i.e. how aggressive would you be with the work-up)?
Here's his CT:

Here's his CT:

Wednesday, December 28, 2005
Abnormal CT scan - part II
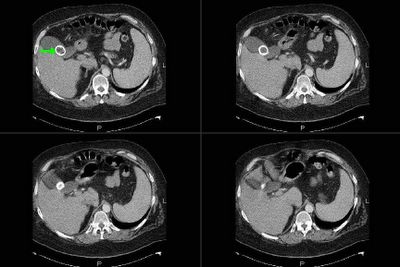
This is the 83 y/o man with the abnormal peripheral lesion. The first post generated an interesting discussion on how old is too old to receive treatment. Since then he has had a PET-CT and a bronch. The lesion looks stable (though only 2 weeks had elapsed) on the CT portion of the PET and there was no abnormal uptake. Hi bronch revealed more airway inflammation on the left bronchial tree than I expected, some Hemophilus but no malignant cells. How would follow him and what would you do next?
Tuesday, December 27, 2005
Patients with treated lung cancer
We see a large number of cases of lung cancer since TN has a rate of TOB use greater than the national average. The American Society of Clinical Oncology does not recommed serial imaging studies for f/up of patients with lung cancer treated with curative intent (lower stages) and there is not very good data on that. How do you usually follow them up?
Wednesday, December 21, 2005
G20210A
Quick question. I have seen this 60 y/o woman in the hospital with B/L pulmonary emboli and DVTs. She has COPD (moderate), OSA and obesity. She was D/C'ed on coumadin and actually received a little over 6 months b/c she underwent a total knee replacement 6 months after the PE. She is now off coumadin, her levels of proteins C&S and ATIII are normal but she is heterozygous for the prothrombin gene mutation at AA 20210. This is a first episode of VTE but she had a lot of clot in her CT with a single genetic defect (no factor V Leiden). Would you recommend indefinite anticoagulation?
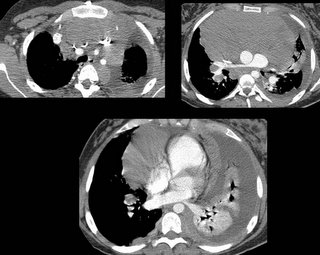
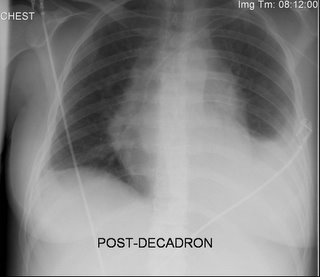
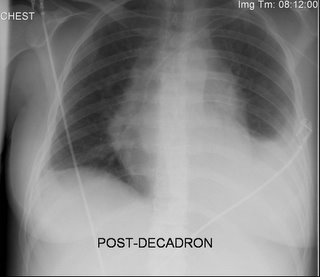
Follow-up to pulmonary infiltrates
This is the 68 y/o man post-ABVD for Hodgkin's described below. He had a bronch this week: bal was cloudy but not purulent or bloody; smears and stains were negative for any organisms, no increase in Eos, no giant cells. TBBx revealed diffuse alveolar damage with edema, an inflammatory infiltrate, no organisms, no lymphoma and changes were consistent with Bleo toxicity. He is still on ABTx and quite hypoxic so we are planning on pulsing him with Solu-medrol.
Tuesday, December 20, 2005
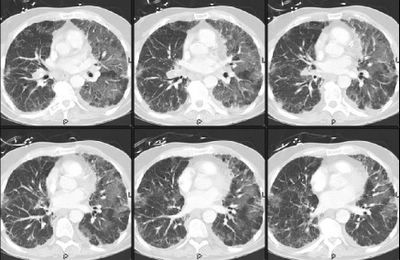
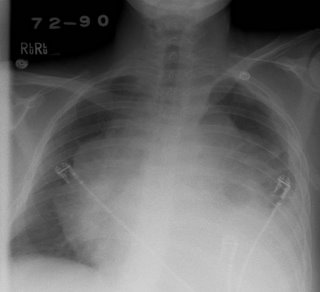
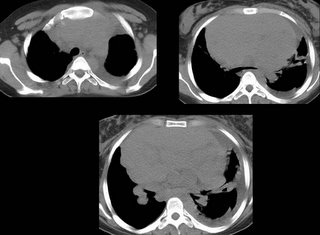
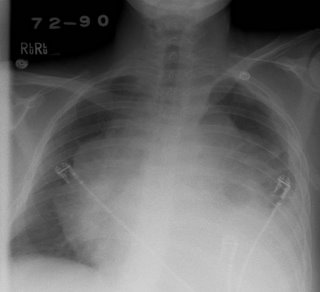
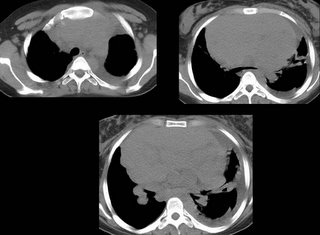
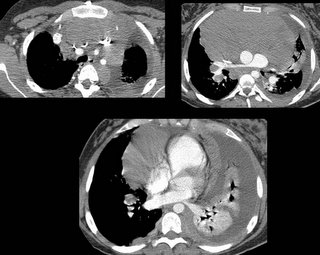
Pulmonary infiltrates
This is a 68 y/o man with a very remote TOB Hx (quit >20 years ago) who had an interesting initial presentation of persistent neck adenopathy since 1995. He had had many non-diagnostic biopsies over the years and was treated for toxo. He finally had an excisional Bx of an 8x6 cm neck node and was found to have Hodgkin's. He had mediastinal adenopathy at the time (7/05) and has received 3 cycles of ABVD. He was set up for another cycle in early December but presented to the hospital with worsening dyspnea, cough (non-productive) and fatigue and was found to be hypoxemic. He is not neutropenic but is quite hypoxic and I have posted his CxR and CT chest below.
What is your DDx and what would you do next?

What is your DDx and what would you do next?

Monday, December 19, 2005
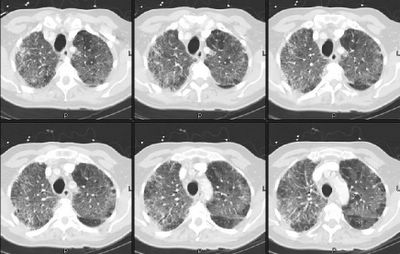
Abnormal CT scan
This is an 83 y/o man sent to us by our CT surgeons. Two months ago he had a tracheo-bronchitis treated by his PCP. A CxR showed a subtle abnormality on his L lung and that was better seen on a CT scan. He is now assymptomatic but has a persistent abnormality on his L lung on a repeat CT scan (see below, this was done roughly 6 weeks after the first one).
He is a former smoker (quit in 1967) with no other remarkable exposures.
Exam is fairly normal.
PFTs showed mild COPD (FEV1~70% with normal TLC, increased RV and DLCO ~60%).
The surgeons thought we might want to see him before cutting anything out.
What would you do next?
He is a former smoker (quit in 1967) with no other remarkable exposures.
Exam is fairly normal.
PFTs showed mild COPD (FEV1~70% with normal TLC, increased RV and DLCO ~60%).
The surgeons thought we might want to see him before cutting anything out.
What would you do next?
Friday, December 16, 2005
Levalbuterol
Our hospital has a very high usage of levalbuterol as opposed to racemic albuterol (most of it actually not motivated by pulmonary). It is often prescribed in higher frequency than the q8 hour use. Pharmacy has been trying to rein this in because of cost differences.
There is a lot of data available (some conflicting) and most of it sponsored by Sepracor (such as Truitt's paper on Chest 2003).
What is your opinion on the use and have you noticed similar patterns with levalbuterol?
There is a lot of data available (some conflicting) and most of it sponsored by Sepracor (such as Truitt's paper on Chest 2003).
What is your opinion on the use and have you noticed similar patterns with levalbuterol?
Thursday, December 15, 2005
Follow up to lung mass
This is the man with the large LUL mass and the hot spot on the sacrum seen on PET. The main question was what to do and how to finish his staging. Our CT surgeon offered to do a mediastinoscopy for further staging (of a IIIA vs IIIB) to help decide on whether he would be operable. He had tumor invasion of the mediastinum itself (T4) with positive N2 nodes (IIIB). We are performing a MRI of the pelvis today to better define that hot spot (his PSA is high too) and a MRI of his head. Since he is not operable we feel inclined to further image but not biopsy the sacral lesion at this point. What do you think?
Wednesday, December 14, 2005
Bronchs and coag's
This comes up fairly often in patients with AFib, mechanical heart valves and liver disease who need bronch's. What is your comfortable cutoff for PT-INR and or platelets when doing a bronchoscopy? Is there any good data on safety and cutoff levels?
Ethical question
69 yo male with PMH of hypertension, CAD and DM2 presented to his PCP with fatigue and "falling asleep anywhere." After testing him for anemia, renal disease and thyroid disease, he decided to get a sleep study. The sleep study was grossly positive with an AHI (RDI) of 67 that occurred with both REM and NREM sleep. During the split night portion of the study, his AHI was reduced to 12 with CPAP of 11 cm H20.
He saw me after the study. When asked, he claimed to fall asleep reading the newspaper in the morning on the weekends, watching TV at night and had, on 2 occassions, fallen asleep while driving. He pulled over, napped for 10 minutes and started to drive again. There were no accidents and he needs to drive each day to get to work. He is constantly sleepy while driving and usually drives with the windows down in 20 degree temperatures to keep himself awake.
From our office, we arranged for CPAP to be delivered to his house the day of his appointment.
Would you ask him not to drive? If so, for how long?
Would you report this to the state (this is not required in the state of Michigan).
He saw me after the study. When asked, he claimed to fall asleep reading the newspaper in the morning on the weekends, watching TV at night and had, on 2 occassions, fallen asleep while driving. He pulled over, napped for 10 minutes and started to drive again. There were no accidents and he needs to drive each day to get to work. He is constantly sleepy while driving and usually drives with the windows down in 20 degree temperatures to keep himself awake.
From our office, we arranged for CPAP to be delivered to his house the day of his appointment.
Would you ask him not to drive? If so, for how long?
Would you report this to the state (this is not required in the state of Michigan).
Tuesday, December 13, 2005
Lung mass
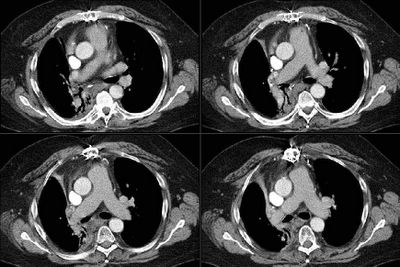
This is a man in his 60's with no previous lung or heart disease. He presented to the ER with atypical R-sided CP, had an abnormal CxR and had the following CT:
I saw him in our office, he has an occasional cough and normal PFTs.
I did a bronch which showed no endobronchial lesions but confirmed a NSCLCa (squamous).
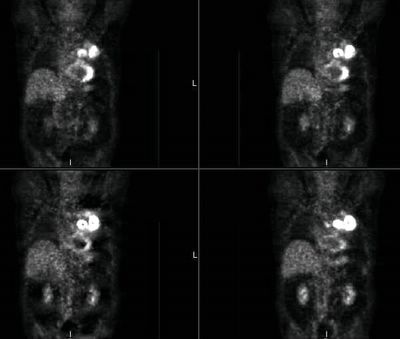
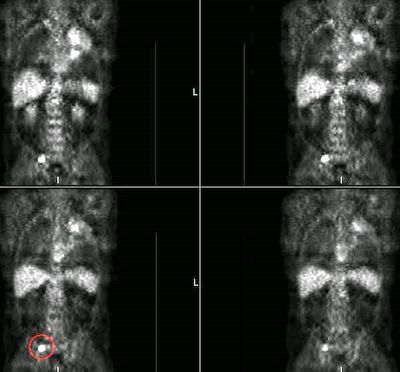
His PET scan showed obvious uptake by the mass and an ipsilateral node.
It also showed some increased uptake in the sacrum:
The sacral area is anterior and not approachable by CT-guided Bx... What would you do next? With the PET but no tissue confirmation from the sacrum would you consider him a stage IV? Would you try and get a surgical Bx from the sacrum?
I saw him in our office, he has an occasional cough and normal PFTs.
I did a bronch which showed no endobronchial lesions but confirmed a NSCLCa (squamous).
His PET scan showed obvious uptake by the mass and an ipsilateral node.
It also showed some increased uptake in the sacrum:
The sacral area is anterior and not approachable by CT-guided Bx... What would you do next? With the PET but no tissue confirmation from the sacrum would you consider him a stage IV? Would you try and get a surgical Bx from the sacrum?
Monday, December 12, 2005
PET and SUV
new comment in unusual configuration cxr. I had a long discussion with the radiologist in nuclear medicine. He essentially refused to tell me the SUV value on a PET scan, saying that there was so much overlap that it was useless. He was not (yet) able to cite any references to back this up but will hopefully be getting back to me on this. Judging by some of the comments here, I gather some of you rely on this value when making decisions regarding the "hotness" of a lesion. While we are awaiting the radiologist's reply, is anyone aware of studies debunking/invalidating the utility of the SUV value?
Friday, December 09, 2005
Follow up to abnormal CT scan
This is the young guy with the mediastinal adenopathy. I did request a PET scan and there was no abnormal uptake anywhere. Mike L raised a good point on that discussion about PET-negative slow growing lymphomas. With these results, what would you do next?
Wednesday, December 07, 2005
rEmerson Biguns
19 year old woman who is 26 weeks pregnant presented with 2 weeks of progressive shortness of breath, which was worse lying down and better sitting up and leaning forward. + wheezing. No fever/chills/sweats. No weight loss. No cough/sputum production.
No past medical history/social history/family history of significance.
The exam was notable only for inspiratory and expriatory wheezing.
No past medical history/social history/family history of significance.
The exam was notable only for inspiratory and expriatory wheezing.
Monday, December 05, 2005
Abnormal CT scan
This is a 44 y/o man referred to our office because of an abnormal CT scan of the chest. He had fallen of a horse and had a CT scan of his thoracic spine and the mediastinal findings were incidental. He has NO respiratory symptoms. He is a smoker (1-1.5 pack/day x ~30years) and has normal PFTs. I have outlined the abnormality on the first cut so you may follow along. No other parenchymal abnormalities were noted.

How would you (or would you) work up this lesion?

How would you (or would you) work up this lesion?
Interesting configuration of a lung lesion.
73-year-old female with mild COPD, former smoker. Found to have a left upper lobe nodule on x-ray:
 A CT scan was performed, confirming a 3 cm vertically oriented cylindrical lesion.
A CT scan was performed, confirming a 3 cm vertically oriented cylindrical lesion.


Do you agree that this is an unusual configuration for a malignancy? Could it be a mucous plug? Well, how about the fact that this is the PET scan results:

 A CT scan was performed, confirming a 3 cm vertically oriented cylindrical lesion.
A CT scan was performed, confirming a 3 cm vertically oriented cylindrical lesion.

Do you agree that this is an unusual configuration for a malignancy? Could it be a mucous plug? Well, how about the fact that this is the PET scan results:

Friday, December 02, 2005
Update on previous lung cancer
There were no comments on this case but I would still like to hear your suggestions since it is an ongoing case and I don't have a final answer yet. This is the 61 y/o man with the previous IIB NSCLCa now with abnormal hilum and RML bronchus with path changes of radiation but no obvious malignancy. As it is getting close to the holidays, he came to the office yesterday for the bronch results and we agreed to watch him closely with a repeat CT in 3 months and no other invasive procedures. What would you do?
Update on lung mass
This is the 54 y/o man with >85p/y of TOB and the PET+ lung mass. We felt that with his pre-test likelihood of malignancy, surgery was his best option. He underwent a LULobectomy with partial resection of ribs as the mass was adherent to them (no bone involvement on the PET-CT) and the frozen was "consistent" with adenoCa. The final path was a granulomatous inflammatory mass with fungal agents consistent with blasto and no cancer.
Update on abnormal CxR and hypoxemia
This is the 58-year-old white male with the ICD, and pulmonary infiltrates. Good pick up on the Amio (I thought about just listin "antiarrhythmics" but that seemed unfair). We followed along the same ideas posted: gentle diuresis, continued BiPAP and then a bronch. He had alveolar spaces filled with foamy macs full of phospholipid complexes. Amio was discontinued and he was placed on steroids. He went to a SNF and eventually came off O2. His PFTs normalized and his CxR cleared up.
Thursday, December 01, 2005
Update on ongoing cases
We have three cases from this week and one question/comment going on and still need to hear from our readers. Try and leave comments/suggestions and we will be posting the conclusions to the lung mass cases tomorrow.
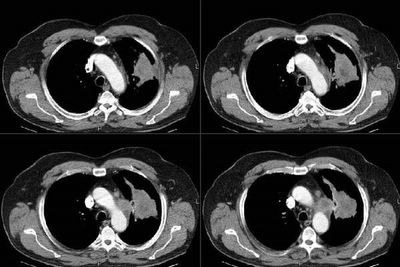
Previous lung cancer
This is a 61 y/o man who was seen in our office last year. He had significant obesity and OSA and was found to have a RUL mass. He underwent resection of a IIB (T2N1M0) NSCLCa (squamous), followed by xRt and chemoTx. His course since then has been remarkable for a fall and a hip Fx but no respiratory problems.
He came back to his PCP this past month with a new cough and R chest tightness. His CT showed some loss of volume and more soft tissue swelling in the hilar area (see below):
Incidentally he had this huge gallstone (cool pic):
I bronch'ed him and he had narrowing and scarring of the residual RML bronchus with normal RLL and a healthy looking RUL stump. EndoBBx, brushings and lavages were remarkable for radiation changes and atypia but no neoplasm. Would you do a PET, a more invasive sampling (e.g. Mediastinoscopy) or just follow him after some ABTx since he has already had maximal therapy to the area and would have limited options with recurrent Ca?
He came back to his PCP this past month with a new cough and R chest tightness. His CT showed some loss of volume and more soft tissue swelling in the hilar area (see below):
Incidentally he had this huge gallstone (cool pic):
I bronch'ed him and he had narrowing and scarring of the residual RML bronchus with normal RLL and a healthy looking RUL stump. EndoBBx, brushings and lavages were remarkable for radiation changes and atypia but no neoplasm. Would you do a PET, a more invasive sampling (e.g. Mediastinoscopy) or just follow him after some ABTx since he has already had maximal therapy to the area and would have limited options with recurrent Ca?
Subscribe to:
Posts (Atom)