Ok--here's an interesting one that I've been following for the past few months. I'm going to present things in steps as they actually unfolded in the evaluation, and let people chime in at each step. So, I'll present some of the information, then stop for comments, then edit the post to include new information, and leave a day or two for more comments. Since this is a Friday afternoon, I won't add new information until Tuesday, so check back.
Here's the case: 26 year old man presented for evaluation of dyspnea for several years. He had been diagnosed with asthma at some point in the past, but had not been on treatment until a few months prior to his presentation. On his initial visit, he was taking a combination short-acting beta-agonist (salbumatol) and inhaled steroid that he had been given while visiting his family in India (he immigrated to the U.S. 4 years ago. He had no acute complaints other than his dyspnea. He had no functional limitation, but noted intermittant wheezing for the past six years (worse with cold or humid weather). Additionally, he had a daily cough productive of "yellow/brown" sputum. The cough is worse in the morning.
His past history, other than the "asthma" was unremarkable until two years ago when he was admitted to a hospital and treated for pneumonia. About a year ago, he saw another pulmonologist who he said didn't really do anything (said pulmonologist called me to say that he had ordered a number of tests, but that the patient never followed up due to a lack of insurance).
Social Hx: Grew up in India, and recently traveled to India for 2 weeks. Smoked 3 packs/week for 5 years, quit one year ago. College educated, works in an office without any known occupational exposures. He has no pets. No family/surgical history. No meds except the combination inhaler. No drug allergies.
On exam, he was a WD/WN man, comfortable, no distress. There was no accessory muscle use. His chest expands symmetrically with inspiration.There is no dullness to percussion or egophony. There are decreased breathsounds noted at the left base along with diffuse inspiratory and expiratorywheezes. There are no rales or rhonchi. The remainder of the exam was normal.
Spirometry: FVC :3.56 (64%) FEV1: 1.78 (41%) FEV1/FVC: 50% There was no significant change following a bronchodilator challenge.
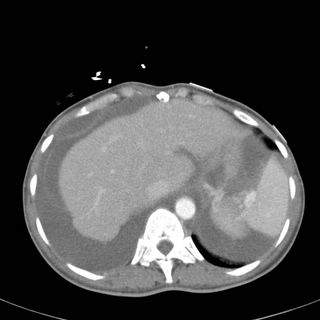
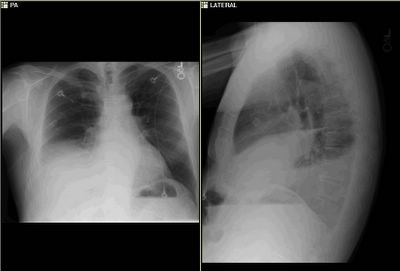
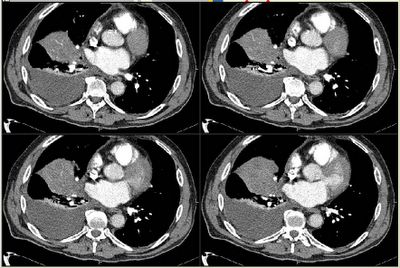
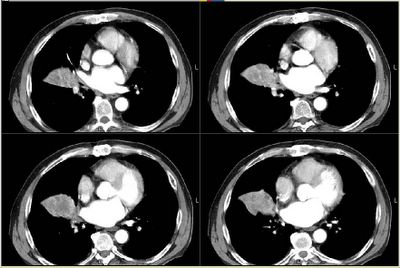
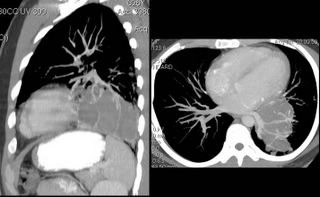
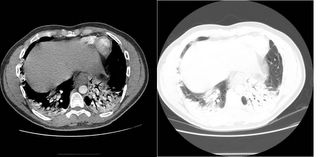
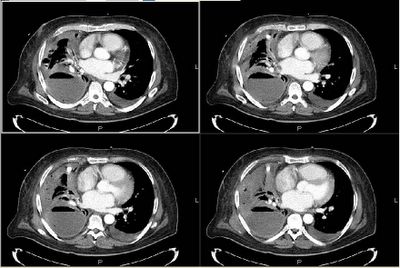
His CXR follows:

Labs: WBC = 9.9 (70% polys, 10% eos) Aspergillus IgG and IgE: normal
This ends the first part of the case: any comments on the CXR, or on diagnostic/therapeutic steps that you would take.
Part 2:
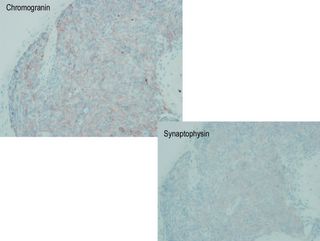
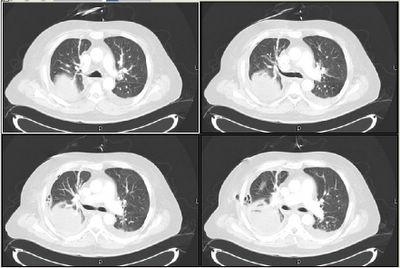
I was called by a prominant chest radiologist before I saw the patient. He told me that the patient had a left lower lobe pneumonia and possibly some central bronchiectasis. So, combined with his spirometry, I obtained studies to evaluate for ABPA (these were negative) and gave a burst and taper of prednisone for his untreated asthma. Because, clinically he had nothing to suggest a pneumonia, I ordered a CT scan.
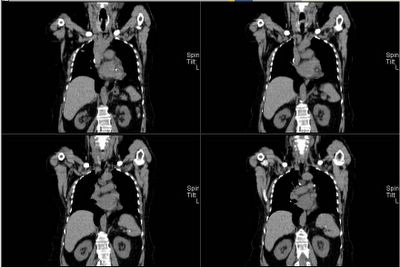
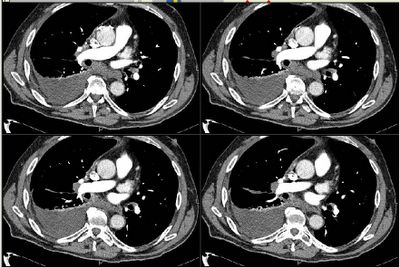
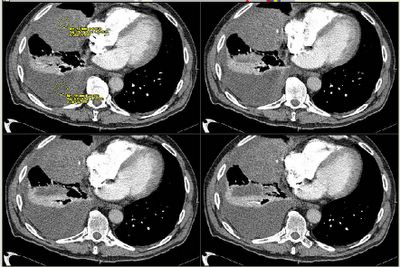
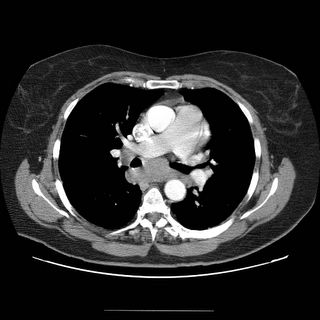
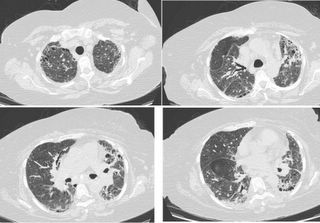
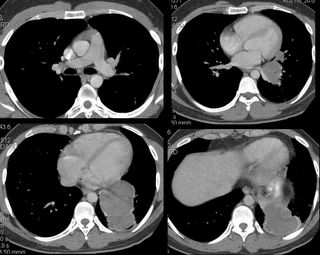
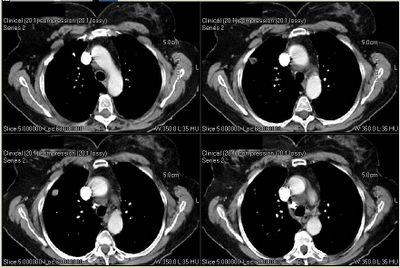
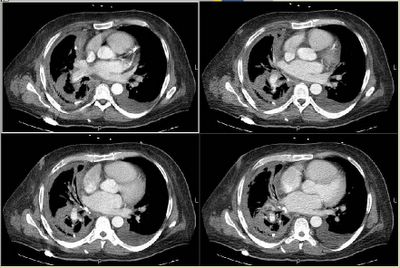
I saw him back in clinic 2 weeks later.His PFT's had improved significantly:FEV1 up to 2.6 L (from 1.78). FVC was unchanged. His TLC was 74% predicted, and his DlCO was normal. His CT scan is shown:
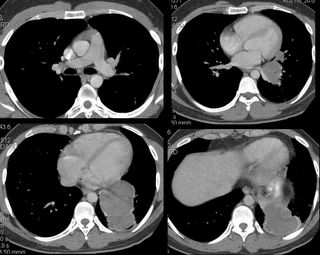
So, now what?
Part 3:
We thought, given the mild eosinophila, his immigration history, and the cystic appearence on CT scan with what appeared to be multiple septae, that this could very well be an echinococcal cyst. Other possibilities included malignancy (esp sarcoma), or sequestration (although we did not identify a feeding vessel). I did not show it, but there was one 2 cm calcified lesion in the liver. So, I presented his case to thoracic surgery for primary resection. Our surgeons asked for an ID opinion, which was obtained. Although review of the literature showed that percutaneous drainage may be an option for hydatid cysts in the liver, this has not been shown in the lung. The ID consultants agreed with primary resection, but we chose to treat for 3 months with albendazole first.
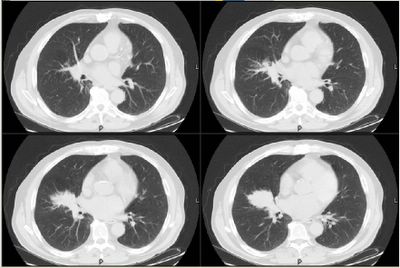
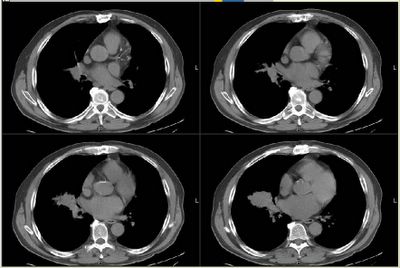
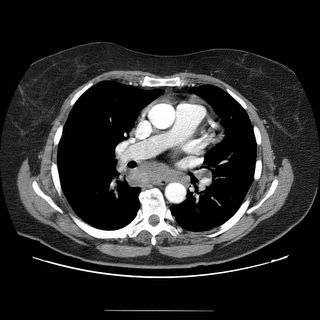
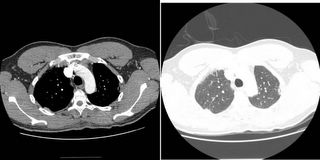
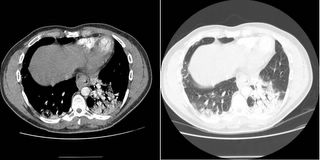
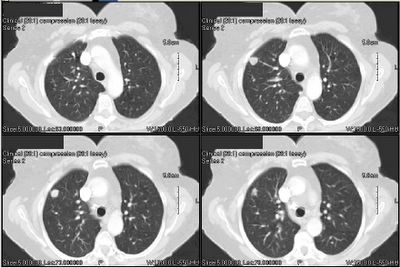
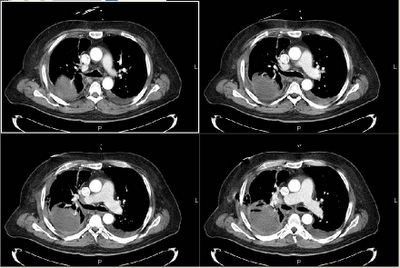
Two weeks later, the story changed again. I was contacted by another radiologist (who had seen the initial CT scan in a conference). She sent me some computer reconstructions:

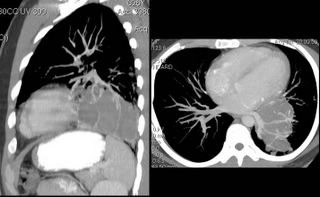
As seen, what we thought were septations were, in fact, vascular branches off of the left pulmonary artery. Additionally, she felt that the fluid density was not cystic (60 hounsfeld units). Now, the possibility of sarcoma came into play.
CONCLUSION: I showed these films to our thoracic surgeon, who again balked, so I rephrased the question. I asked him to name any potential diagnosis of this lesion for which resection was not appropriate management. The patient was taken to the OR 2 weeks later, and a left lower lobectomy was done.
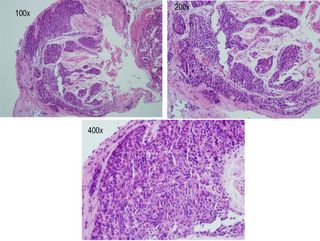
Gross Path: multiple cystic lesions containing "thick green and brown material."
Microscopic Diagnosis: bronchiectasis with eosinophilic abscesses.
There were no parasites seen. There was no fungus. Cultures were negative.
I saw the patient in follow-up last week, and we are both dissapointed at the lack of a definitive etiology for all of this. He feels well, although he stopped taking his meds and his airways obstruction has significantly worsened. He is off of the albendazole, and we have chosen to follow-up clinically and with periodic imaging to identify any potential new lesions at an early timepoint.
Any other comments, thoughts, or suggestions?