One of my COPD patients was asking me about purchasing a portable/travel concentrator such as this one.
Have you had much experience or feedback with portable oxygen concentrators?
Wednesday, December 27, 2006
Tuesday, December 19, 2006
Vocal cord paralysis
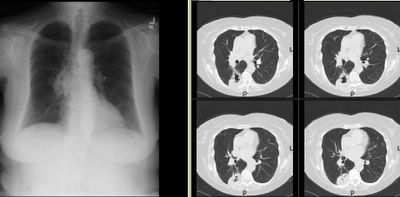
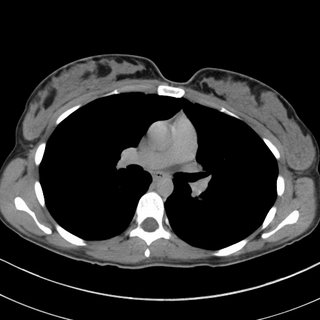
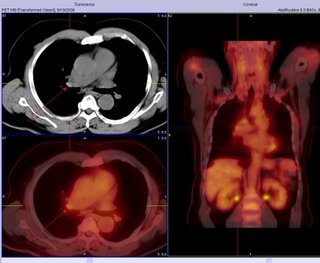
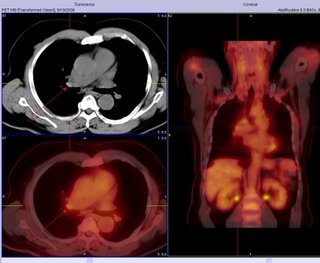
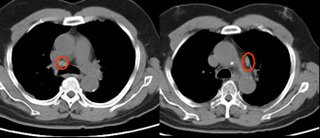
This 61 y/o man was sent to our office by ENT for w/up of a vocal cord paralysis. He has had subacute-onset hoarseness for the past 2-3 months and ENT found a unilateral R vocal cord paralysis. He did a CT (see the images below), which only showed some mediastinal and hilar (R>L) adenopathy much of which is calcified.
He has had a PET scan which showed some very faint (SUV<4) style="display: block; text-align: center;" alt="" src="http://photos1.blogger.com/x/blogger/7040/842/320/933316/Vocal.jpg" border="0">
He has had a PET scan which showed some very faint (SUV<4) style="display: block; text-align: center;" alt="" src="http://photos1.blogger.com/x/blogger/7040/842/320/933316/Vocal.jpg" border="0">
Friday, December 15, 2006
RLS
Have you had a lot of experience with Requip (ropinirole) for restless leg syndrome?
If not, what is your preferred therapy fro RLS?
If not, what is your preferred therapy fro RLS?
Monday, December 11, 2006
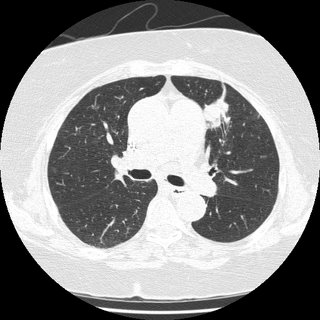
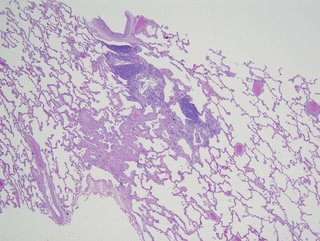
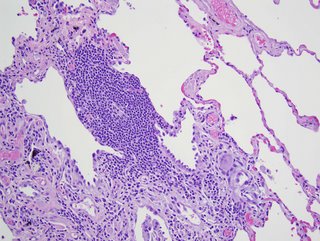
Differential and w/w
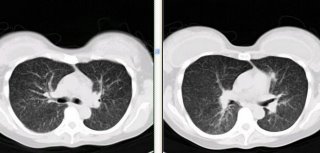
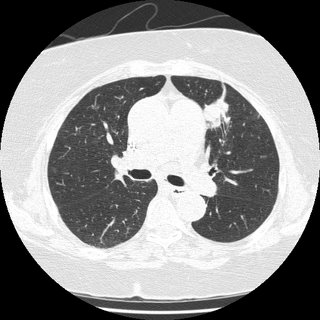
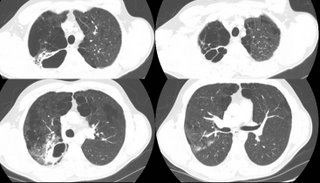
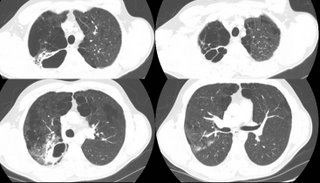
43 year old presented with 6 weeks of progressive dyspnea associated with URI-type symptoms. Had recieved several courses of antibiotics as an outpatient. No fever/chills. + non-productive cough. No associated s/s. Non-smoker. No occupational exposure. On presentation, he was hypotensive, but alert and oriented. His was quite comfortatble despite profound hypoxia (initial oxygen saturation of 62% on room air). Physical exam has some scattered rales. WBC is 4, without a shift. Blood count and platelets are normal. He is hypoxic, requiring up to 100% supplemental oxygen by non-rebreather to maintain a pO2 in the 60's. His ventilation is adequate, with a pCO2 of 42 and a pH of 7.39.
A CT scan shows:



A CT scan shows:



Saturday, December 09, 2006
Follow-up to Pulmonary Nodules
This is the 51 y/o woman with COPD and pulmonary nodules.
We had the same concerns and DDx as proposed in the discussion. I did a bronchoscopy and we got good samples consistent with RB-ILD.
She was counselled again regarding TOB cessation and agreed to try varenicline. She will follow-up in a few weeks and we will monitor her CxR and PFTs.
We had the same concerns and DDx as proposed in the discussion. I did a bronchoscopy and we got good samples consistent with RB-ILD.
She was counselled again regarding TOB cessation and agreed to try varenicline. She will follow-up in a few weeks and we will monitor her CxR and PFTs.
Tuesday, December 05, 2006
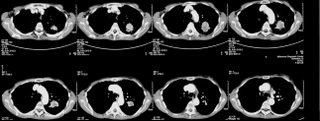
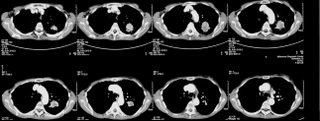
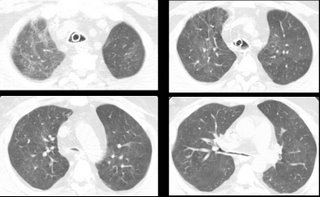
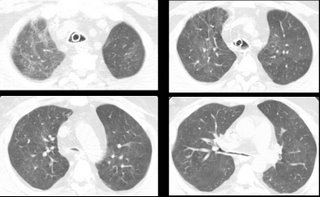
Pulmonary nodules
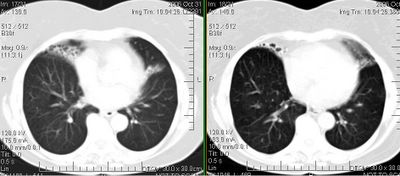
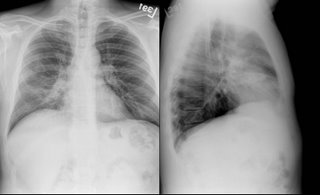
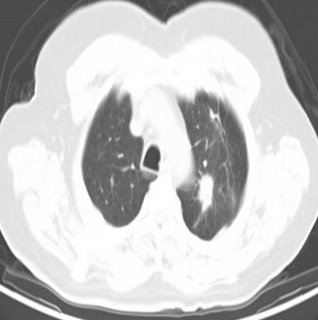
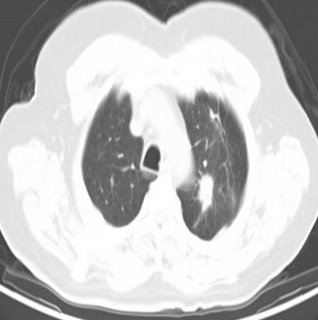
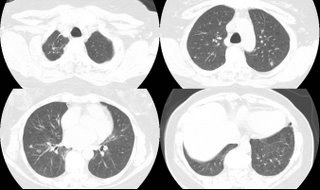
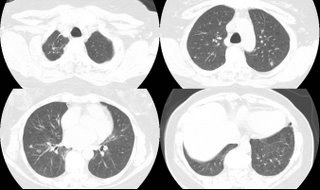
 This is a 51 y/o woman followed in our office for moderate COPD. She continues to smoke and has had worsening dyspnea and weight loss for a couple months. Her CxR and CT scan, which in the past showed hyperinflation and nothing else, now have these pulmonary nodules.
This is a 51 y/o woman followed in our office for moderate COPD. She continues to smoke and has had worsening dyspnea and weight loss for a couple months. Her CxR and CT scan, which in the past showed hyperinflation and nothing else, now have these pulmonary nodules.What is your DDx and wht would you do next?

Thursday, November 30, 2006
Airway remodelling
I have posted a question on this a while ago. I see a fair number (just saw one today) of older patients (usually women) who have never smoked, have normal gas exchange and chest radiography but who present with moderately severe degrees of fixed obstructive lung disease. They never have any history of asthma, cough or wheezing and their only complaint is DOE.
Usually there is some small-airway obstruction on the expiratory images of a HRCT but no other structural abnormalities.
Have you seen much of that? How do you label these patients? Unsuspected asthma with remodelling?
Usually there is some small-airway obstruction on the expiratory images of a HRCT but no other structural abnormalities.
Have you seen much of that? How do you label these patients? Unsuspected asthma with remodelling?
Monday, November 27, 2006
SOB
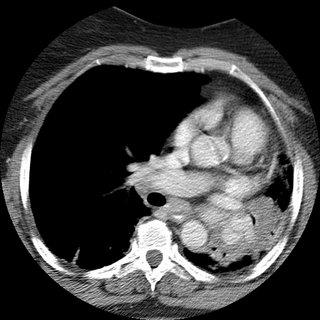
62 woman c/o 2 weeks ago started to have cough with greenish sputum. She presented to the ER where workup included a CT (below).
Pt states that was diagnosed with asthma in 2002; at that time she had a CXR that showed scar tissue in the left upper lobe secondary to a previous pneumonia.
She noticed that over the last year, she has being unable to lay down over her right side because she would feel short of breath, so that she always sleep over her left side. Denies frequent cough, sputum production, hemoptysis, weight loss, loss of appetite, chronic chest pain.
SOCIAL HISTORY:
pt has 40 pack year history of smoking, quit in 1998. She works as hair stylist and is exposed to fumes and chemicals. Denies exposure to TB. No recent travels.
PHYSICAL EXAM:
BP 139/83, HR 86x', RR 16x', O2Sat 93% on RA, W 212 pounds.
Patient is awake, alert, obese, oriented x3, no acute distress.
Neck, no lymphadenomegaly. Chest, no use of accesory muscles, no retractions, flat to percussion on the left, no prolonged expiration, absent breath sounds in the left, no wheezes, no crackles. CV: regular rhythm, no S3 or S4, no murmurs. No rubs.
Spirometry showed severe obstruction.
(quick) DDx and how would you proceed?
Pt states that was diagnosed with asthma in 2002; at that time she had a CXR that showed scar tissue in the left upper lobe secondary to a previous pneumonia.
She noticed that over the last year, she has being unable to lay down over her right side because she would feel short of breath, so that she always sleep over her left side. Denies frequent cough, sputum production, hemoptysis, weight loss, loss of appetite, chronic chest pain.
SOCIAL HISTORY:
pt has 40 pack year history of smoking, quit in 1998. She works as hair stylist and is exposed to fumes and chemicals. Denies exposure to TB. No recent travels.
PHYSICAL EXAM:
BP 139/83, HR 86x', RR 16x', O2Sat 93% on RA, W 212 pounds.
Patient is awake, alert, obese, oriented x3, no acute distress.
Neck, no lymphadenomegaly. Chest, no use of accesory muscles, no retractions, flat to percussion on the left, no prolonged expiration, absent breath sounds in the left, no wheezes, no crackles. CV: regular rhythm, no S3 or S4, no murmurs. No rubs.
Spirometry showed severe obstruction.
(quick) DDx and how would you proceed?
Friday, November 24, 2006
Follow-up to dyspnea
This is the recent post of the 47 y/o woman with dyspnea. JJ and Krayem suggested HP and on the TBBx we had loose granulomata with lots of lymphocytes and negative organisms on stains and Cxs. The pathologist felt quite confident calling it as HP. Unfortunately I don't know what is the culprit exposure yet...
Tuesday, November 21, 2006
CXR followup after resection
A curious reader from Maine would like to know:
How frequently and for how long, do you follow xray/CT's after the surgical resection of a stage 2 lung cancer.
How frequently and for how long, do you follow xray/CT's after the surgical resection of a stage 2 lung cancer.
BCG and latent tb
A patient had a previous negative PPD as a requirement for work. She then went oversees for a time and receieved the BCG vaccine. She is now back in this country and as part of work requirements gets another PPD which is now positive. She is asymptomatic and the chest xray is negative.
How would you handle this?
How would you handle this?
Dyspnea

 I have just seen this 47 y/o woman for new onset dyspnea. She has had malaise, non-productive cough and DOE for the past 6 weeks. Occasional "low-grade" temps but no fevers.
I have just seen this 47 y/o woman for new onset dyspnea. She has had malaise, non-productive cough and DOE for the past 6 weeks. Occasional "low-grade" temps but no fevers.No TOB Hx. She works at a auto air-bag manufacturer and part-time at a Wal-Mart. No other exposures. Exam is pretty unremarkable. PFTs revealed a mild restrictive deffect with low DLCo.
Any suggestions? (BTW, ignore the small apical PTx, that was from vigorous bronching).

Wednesday, November 15, 2006
Dyspnea
I just saw this 70 y/o woman in consult today. Her only complaint is dyspnea on exertion: she gets tired after walking more than a mile. No TOB, no Hx of lung Dz.
She had 3-4 episodes of pneumonia within 2 years > 5years ago.
No childhood illnesses.
No chronic cough. Physical exam is unremarkable. PFTs showed a moderate mixed defect.
She has the bronchiectatic/focal cystic changes above and the rest of the CT was normal.
How would you work up her focal bronchiectasis and do think those small areas are sufficient explanation to her dyspnea.
Diagnostic dilemna
Ok, hopefully you can help me with this case. It's fairly long and complicated - not easy in this blog format but that's what we're stuck with. I presented this case before, but that was before some additional data.
He is a 45 year old with 6 months of a cough. This was found on a CT scan:

A biopsy was done. It showed interstitial inflammation. A previous biopsy had been obtained with similar non-specific findings. That one was read as "a mixed inflammatory infiltrate, greatest in the bronchial submucosa, with increased numbers of eosinophils. There are intraalveolar pigment/ hemosiderin laden macrophages and fresh blood; there is no vasculitis in this limited sample. Grocott stain is negative for fungus."
Also, a 2.1 x 1.3 cm hypoattenuating lesion was found within the tail of the
pancreas, nonspecific. This was biopsied by CT-guided and showed "The biopsy has stromal fibrosis, attenuation of the ducts/ acinar component and accentuation of the islets. In one level, there is a single granuloma My underline and the possibility of an underlying granulomatous inflammatory disease, such as a fungal infection or tuberculosis, accounting for both the lung and pancreatic lesions, cannot be excluded. Grocott stain is negative for fungus. Ziehl-Neelsen stain is negative for acid-fast bacteria. Immunostain is negative for mycobacteria. The present biopsy is not representative of a mass lesion."
He also was found to have adrenal insufficiency (cort-stim test) picked up when he presented to my clinic with hypotension, hyponatremia and hyperkalemia. (ACTH was 356). He also had a calcium of 10.9 but with normal PTH level (23).
Bronchial washings were negative for fungal. There was no growth of any micro subsequently.
A p-ANCA and c-ANCA were negative.
Any ideas on what's going on with this patient?
He is a 45 year old with 6 months of a cough. This was found on a CT scan:

A biopsy was done. It showed interstitial inflammation. A previous biopsy had been obtained with similar non-specific findings. That one was read as "a mixed inflammatory infiltrate, greatest in the bronchial submucosa, with increased numbers of eosinophils. There are intraalveolar pigment/ hemosiderin laden macrophages and fresh blood; there is no vasculitis in this limited sample. Grocott stain is negative for fungus."
Also, a 2.1 x 1.3 cm hypoattenuating lesion was found within the tail of the
pancreas, nonspecific. This was biopsied by CT-guided and showed "The biopsy has stromal fibrosis, attenuation of the ducts/ acinar component and accentuation of the islets. In one level, there is a single granuloma My underline and the possibility of an underlying granulomatous inflammatory disease, such as a fungal infection or tuberculosis, accounting for both the lung and pancreatic lesions, cannot be excluded. Grocott stain is negative for fungus. Ziehl-Neelsen stain is negative for acid-fast bacteria. Immunostain is negative for mycobacteria. The present biopsy is not representative of a mass lesion."
He also was found to have adrenal insufficiency (cort-stim test) picked up when he presented to my clinic with hypotension, hyponatremia and hyperkalemia. (ACTH was 356). He also had a calcium of 10.9 but with normal PTH level (23).
Bronchial washings were negative for fungal. There was no growth of any micro subsequently.
A p-ANCA and c-ANCA were negative.
Any ideas on what's going on with this patient?
Tuesday, November 14, 2006
LUL nodule with ipsilateral LAD
25 yo female with no PMH presents with above.
She was well until April when she travelled to Phoenix to visit friends. When she returned, she had a bad URI. Her PCP obtained a CXR which showed a shadow in the L hilum, and a CT was recommended.
The CT was from an OSH and resembles the CT shown below. The L hilar fullness is a node clearly visualized in the OSH CT; the CT I show is without contrast (she got hives after the first CT). The rec on the CT was to obtain a repeat in 3 months. This is the 3 month CT.
She is currently asymptomatic other than a 20 lb weight loss since 4/06. She has not changed her eating habits or exercising habits.
PMH: Non-smoker but moderate second-hand smoke from her parents.

Labs: CBC, chemistries, U/a are all normal.
What would you do?
She was well until April when she travelled to Phoenix to visit friends. When she returned, she had a bad URI. Her PCP obtained a CXR which showed a shadow in the L hilum, and a CT was recommended.
The CT was from an OSH and resembles the CT shown below. The L hilar fullness is a node clearly visualized in the OSH CT; the CT I show is without contrast (she got hives after the first CT). The rec on the CT was to obtain a repeat in 3 months. This is the 3 month CT.
She is currently asymptomatic other than a 20 lb weight loss since 4/06. She has not changed her eating habits or exercising habits.
PMH: Non-smoker but moderate second-hand smoke from her parents.

Labs: CBC, chemistries, U/a are all normal.
What would you do?
Monday, November 13, 2006
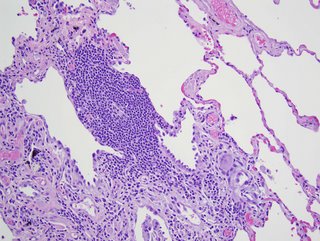
Sarcoidosis and weight loss
A 40 year old affrican american man presented with a 40 lb weight loss and a slight cough. His spirometry was normal. A CXR showed symmetrical bilateral hilar adenopathy and a transbronchial biopsy of the upper lung showed noncaseating granulomas, consistent with sarcoid. He has no complaints of shortness of breath.
Would you treat with steroids? Is there any caveats or different management decisions regarding sarcoid, when the only presenting abnormality is weight loss (SOB absent with normal PFTs).
Would you treat with steroids? Is there any caveats or different management decisions regarding sarcoid, when the only presenting abnormality is weight loss (SOB absent with normal PFTs).
Tuesday, November 07, 2006
ICS in the hospital
What is your usual practice regarding inhaled steroids when you admit a patient for either status asthmaticus or AECB?
If they are already on an ICS on admission and they will be on a systemic steroid do you continue the ICS?
Conversely, if they are not on an ICS on admission and are now on a systemic steroid, do you start an ICS during the admission or after D/C?
If they are already on an ICS on admission and they will be on a systemic steroid do you continue the ICS?
Conversely, if they are not on an ICS on admission and are now on a systemic steroid, do you start an ICS during the admission or after D/C?
Friday, November 03, 2006
preop stage
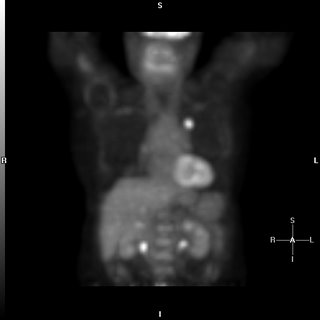
I thought this was an interesting case because it involves role and possible limitations of PET scanning for staging prior to surgical resection. A 69 year old presented with a LUL mass. The bronch brushings revealed non-small cell lung cancer. A PET showed the intense uptake in that mass:

The PET was otherwise negative except for some mild hypermetabolic activity in the right hilar and pericarinal regions corresponding to nonenlarged lymph nodes on CT:
Because of this, he underwent LUL lobectomy. However, an ipsilateral mediastinal node was positive. I do not think they sampled the area of the hilum that lit up (it was contralateral), so in this case the PET did not indicate that he had spread. Also of interest, the margins from resected mass were negative.

The PET was otherwise negative except for some mild hypermetabolic activity in the right hilar and pericarinal regions corresponding to nonenlarged lymph nodes on CT:
Because of this, he underwent LUL lobectomy. However, an ipsilateral mediastinal node was positive. I do not think they sampled the area of the hilum that lit up (it was contralateral), so in this case the PET did not indicate that he had spread. Also of interest, the margins from resected mass were negative.
Thursday, November 02, 2006
Sticks and (bronchial) stones...
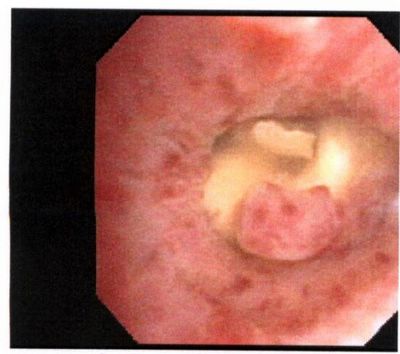
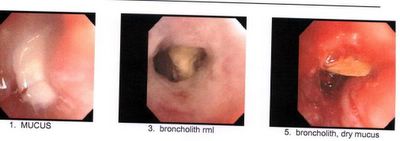
My partner bronch'ed this pleasant 78 y/o woman with no TOB Hx who had developed a persistent RML collapse. The first picture was taken while instilling NSS to keep the airway open.
The lesion was hard to biopsy and there was purulent mucus behind it.
The second set of pictures was a re-bronch 2-3 days later after he tried to remove as much as possible with the forceps.
Any suggestion, comments?
Wednesday, November 01, 2006
Follow-up to Abnormal CxR
This is my VIP patient who got to see us and Hem-Onc at the same time and had a Squam on a CT-guided Bx.
She then had a PET scan which lit up on the mass and on a small (<1 cm) ipsilateral hilar lymph node.
She underwent a med which showed only reactive adenopathy. She had a lobectomy 2 days ago with a T2 squam with negative margins and negative nodes.
At your institution, would you offer adjuvant chemo, xRt, both or neither at this point?
She then had a PET scan which lit up on the mass and on a small (<1 cm) ipsilateral hilar lymph node.
She underwent a med which showed only reactive adenopathy. She had a lobectomy 2 days ago with a T2 squam with negative margins and negative nodes.
At your institution, would you offer adjuvant chemo, xRt, both or neither at this point?
Monday, October 30, 2006
Follow up to the 66 year old with tree in bud
This woman had presented with hemoptysis once and a CT scan showed tree in bud pattern and some nodularity. She presented a year later with cough and sputum. A culture had previously shown 1/3 AFB + but non-TB and non-avium. Her symptoms are the daily cough without constitutional symptoms and no shortness of breath.
I sent off a sputum and it showed Many PMNs, few Epithelial cells, many Gram positive cocci in pairs, chains and clusters and rare Gram negative bacilli.
What would you do now?
I sent off a sputum and it showed Many PMNs, few Epithelial cells, many Gram positive cocci in pairs, chains and clusters and rare Gram negative bacilli.
What would you do now?
The Philosophy of Disclosure
From AK:
I'm sure most of us have seen some close variation on this clinical theme: a smoker has a suspicious lung mass with evidence of metastasis elsewhere, and you're consulted to help get tissue. The patient hasn't seen the scans, doesn't know the overwhelming odds that they have metastatic lung cancer. As a consultant, how much should you tell the patient before you have path results? If they ask about the possibility of surgical resection, is it right to put off an answer you know is highly likely to be correct?
I'm sure most of us have seen some close variation on this clinical theme: a smoker has a suspicious lung mass with evidence of metastasis elsewhere, and you're consulted to help get tissue. The patient hasn't seen the scans, doesn't know the overwhelming odds that they have metastatic lung cancer. As a consultant, how much should you tell the patient before you have path results? If they ask about the possibility of surgical resection, is it right to put off an answer you know is highly likely to be correct?
Thursday, October 26, 2006
Lung cancer screening
The International Early Lung Cancer Action Program Investigators published the results from CT screening >30,000 patients with chest CTs in today's NEJM.
They found a shift towards picking up more early stage disease.
Have you had a chance to see the study? How do you think this will affect our practice?
They found a shift towards picking up more early stage disease.
Have you had a chance to see the study? How do you think this will affect our practice?
Wednesday, October 25, 2006
Treatment of GERD
How do you make a determination to treat for GER in patients with asthma?
There is some data available saying that treatment may reduce exacerbations and improve quality of life...
Littner MR, Leung FW, Ballard ED 2nd, Huang B, Samra NK; Lansoprazole Asthma Study Group.
Effects of 24 weeks of lansoprazole therapy on asthma symptoms, exacerbations, quality of life, and pulmonary function in adult asthmatic patients with acid reflux symptoms.
Chest. 2005 Sep;128(3):1128-35.
PMID: 16162697 [PubMed - indexed for MEDLINE]
There is some data available saying that treatment may reduce exacerbations and improve quality of life...
Littner MR, Leung FW, Ballard ED 2nd, Huang B, Samra NK; Lansoprazole Asthma Study Group.
Effects of 24 weeks of lansoprazole therapy on asthma symptoms, exacerbations, quality of life, and pulmonary function in adult asthmatic patients with acid reflux symptoms.
Chest. 2005 Sep;128(3):1128-35.
PMID: 16162697 [PubMed - indexed for MEDLINE]
Preop eval for secondary HTN due to severe COPD
Redneck pulmonologist submits this question:
Would you do anything for secondary pulmonary hypertension (estimated PAP of 80-90 mmHG on echo) due to COPD before undergoing renal transplant? Her COPD is 2 to AAT deficiency and stable on AAT replacement. FEV1 of 40% predicted. She has documented nocturnal desat on sleep study without significant sleep apnea. But she is non-compliant with home O2. Daytime sat on RA is OK. She is not a smoker. She is on dialysis and her ESRD is due to pauci-immune vasculitis and has been treated with steroids and Cellcept. Work up for other causes of secondary pulmonary HTN is negative.
Would you do anything for secondary pulmonary hypertension (estimated PAP of 80-90 mmHG on echo) due to COPD before undergoing renal transplant? Her COPD is 2 to AAT deficiency and stable on AAT replacement. FEV1 of 40% predicted. She has documented nocturnal desat on sleep study without significant sleep apnea. But she is non-compliant with home O2. Daytime sat on RA is OK. She is not a smoker. She is on dialysis and her ESRD is due to pauci-immune vasculitis and has been treated with steroids and Cellcept. Work up for other causes of secondary pulmonary HTN is negative.
Tuesday, October 24, 2006
Is this BOOP, Y-J?
41 yo male who works for a satellite dish installation company presented with progressive dyspnea over a couple of months. An urgent care CXR was (+) for a nodule in the R mid lung field, and he was referred to his PCP; he received no intervention at that time. He was lost to f/u and ultimately presented with progressive symptoms one month later. His PCP obtained a CT (see below) and he was sent to be admitted. Upon seeing him, he look chronically ill, but not toxic.

I bronched him, and it was non-diagnostic. I sent him for a surgical biopsy.
The report was read as BOOP with an microscopic sulfur granules c/w actinomycosis.
I started him on Augmentin and saw in the office in 3 weeks.
He was no better. Spiro was c/w were moderate restrictive vent defect.
So, I started him on steroids at 40 mg/day of prednisone x 3 weeks then 30 mg/day.
I saw him 4 weeks later (about 1 week into his 30 mg/day) without any clinical improvement.
His full PFT's are c/w mild obstruction with air trapping and impaired gas exchange (DL ~70% predicted). He is a smoker, and is still smoking about 1/2 ppd.
I had his biopsy reviewed by Jeff Myers at U of M (profoundly smart and helpful- wish he would have joined the faculty 5 years sooner), but he thought the original interp was correct.
Now what?

I bronched him, and it was non-diagnostic. I sent him for a surgical biopsy.
The report was read as BOOP with an microscopic sulfur granules c/w actinomycosis.
I started him on Augmentin and saw in the office in 3 weeks.
He was no better. Spiro was c/w were moderate restrictive vent defect.
So, I started him on steroids at 40 mg/day of prednisone x 3 weeks then 30 mg/day.
I saw him 4 weeks later (about 1 week into his 30 mg/day) without any clinical improvement.
His full PFT's are c/w mild obstruction with air trapping and impaired gas exchange (DL ~70% predicted). He is a smoker, and is still smoking about 1/2 ppd.
I had his biopsy reviewed by Jeff Myers at U of M (profoundly smart and helpful- wish he would have joined the faculty 5 years sooner), but he thought the original interp was correct.
Now what?
tree in bud in a 66 year old.
66-year-old lady who presented initially to our Pulmonary Clinic 2 years ago for evaluation of a one-time episode of hemoptysis. A CT of her chest showed focal areas of local bronchiectasis, tree-in-bud pattern. There was a concern about atypical mycobacteria and sputum cultures were obtained. Only one of those was positive for
non tuberculous mycobacteria. Since she was asymptomatic she was merely followed. A year later she has a bit of a nagging cough but no constitutional symptoms. However, a follow-up chest CT showed decrease in the nodularity in the outer lower
aspect of the right upper lobe, but increased atelectasis
and thickening around several bronchi the areas in the medial segment
of the right middle lobe.
In terms of management, how would you proceed, given the slight worsenening radiographically?
non tuberculous mycobacteria. Since she was asymptomatic she was merely followed. A year later she has a bit of a nagging cough but no constitutional symptoms. However, a follow-up chest CT showed decrease in the nodularity in the outer lower
aspect of the right upper lobe, but increased atelectasis
and thickening around several bronchi the areas in the medial segment
of the right middle lobe.
In terms of management, how would you proceed, given the slight worsenening radiographically?
Friday, October 20, 2006
Follow-up to "What is wrong with this picture?"
I thought this was pretty interesting CT scan...
This patient has congenital atresia of the R pulmonary artery with absent R pulmonary circulation (this was a CT-A so you can see some opacified vessels on the L but none on the R). He likely only has some systemic (bronchial) circulation on the R. He has no pulm HTN on ECHO (no surprise, people do survive pneumonectomies) but we counselled him strongly on smoking cessation...
This patient has congenital atresia of the R pulmonary artery with absent R pulmonary circulation (this was a CT-A so you can see some opacified vessels on the L but none on the R). He likely only has some systemic (bronchial) circulation on the R. He has no pulm HTN on ECHO (no surprise, people do survive pneumonectomies) but we counselled him strongly on smoking cessation...
Wednesday, October 18, 2006
Diagnosis and management questions
Get some feedback from others: Submit a case! If there are too many details (i.e. time consuming), feel free to submit a brief one and people can ask for clarifications in the comments.
Tuesday, October 17, 2006
Abnormal CxR
I usually don't like those boards-type question that ask "what would you do next?" and only let you choose one option since we often do more than one thing in real life.
Having said that, I am curious as to what you would do next in this case. This is kind of a VIP patient so she was referred to a couple different specialists at the same time.
She is in her early 70s, quit smoking in 1972, near normal PFTs (FEV1~70%, normal DLCO) and has an abnormal CxR. It started as an URI and then she developed a "deeper" cough with purulent sputum production and some pleuritic CP.
The abnormal CxR (and some CT cuts) are shown below.
She had no adenopathy on the CT.
What would be your first step?
Having said that, I am curious as to what you would do next in this case. This is kind of a VIP patient so she was referred to a couple different specialists at the same time.
She is in her early 70s, quit smoking in 1972, near normal PFTs (FEV1~70%, normal DLCO) and has an abnormal CxR. It started as an URI and then she developed a "deeper" cough with purulent sputum production and some pleuritic CP.
The abnormal CxR (and some CT cuts) are shown below.
She had no adenopathy on the CT.
What would be your first step?
Monday, October 16, 2006
Shortness of breath
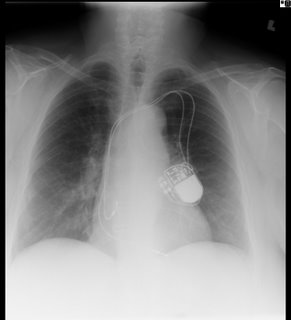
79-year-old man who underwent a four-vessel CABG in January 2006. A few months prior to that, he had developed some malaise and ultimately chest pain leading to an angiogram that revealed 95%, 90%, 80%, and 60% occlusion. After the 4-vessel CABG, he reports shortness of breath worse in the supine position that occurs quite quickly after lying down, perhaps after a minute.
He is able to walk a few miles without significant shortness of breath. He is also able to walk up a flight of stairs with only moderate shortness of breath, and he denies any muscle weakness or achiness. He is able to stand from the sitting position in the chair with a bit of shortness of breath, but no frank weakness. The patient denies any fevers, chills, or night sweats. Furthermore, he denies a cough. There is no productive cough except for the occasional cold about once a year. Rest of his complete review of systems is noncontributory.
On exam it is unremarkable with good air entry bilaterally. In the supine position there is bilateral paradoxical abdominal movement with inspiration.
A CXR is here:
I obtained spirometry in the supine position and repeated that in the upright:
FVC Upright: 2.61L (64% predicted)
Supine: 1.18L (29% predicted) -55% change in vital capacity
PI max cmH2O (51%) 100
PE max cmH2O (104%) 187
It appears he has bilateral diaphragmatic paralysis. It coincides with the CABG, but I think this would be fairly atypical, as that is usually associated with unilateral. In terms of muscle weakness, the low PI but normal PE max argues against this.
Thoughts?
He is able to walk a few miles without significant shortness of breath. He is also able to walk up a flight of stairs with only moderate shortness of breath, and he denies any muscle weakness or achiness. He is able to stand from the sitting position in the chair with a bit of shortness of breath, but no frank weakness. The patient denies any fevers, chills, or night sweats. Furthermore, he denies a cough. There is no productive cough except for the occasional cold about once a year. Rest of his complete review of systems is noncontributory.
On exam it is unremarkable with good air entry bilaterally. In the supine position there is bilateral paradoxical abdominal movement with inspiration.
A CXR is here:
I obtained spirometry in the supine position and repeated that in the upright:
FVC Upright: 2.61L (64% predicted)
Supine: 1.18L (29% predicted) -55% change in vital capacity
PI max cmH2O (51%) 100
PE max cmH2O (104%) 187
It appears he has bilateral diaphragmatic paralysis. It coincides with the CABG, but I think this would be fairly atypical, as that is usually associated with unilateral. In terms of muscle weakness, the low PI but normal PE max argues against this.
Thoughts?
Wednesday, October 11, 2006
Follow up to change in mental status
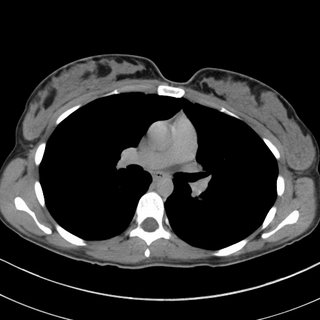
This patient presented with change in MS. The CXR had shown some patchy markings but nothing specific. But the right hilar was full-looking so a CT was done:

Lung windows:

Thoughts?

Lung windows:

Thoughts?
Tuesday, October 10, 2006
Persistent pleural effusion
This is a 38 year old man who is 1.5 years s/p a bone marrow transplant for non-Hodgekin's Lymphoma that had relapsed despite several chemotherapeutic regimens. His post-transplant course has been generally uneventful, with good engraftment, no major infectious complications, and minimal GVHD of the skin and gut. He also had a DVT at some point, treated with adequate anticoagulation for 9 months. He was referred for a right pleural effusion. This was tapped-it was a chylothorax. Flow-cytometry was negative for a recurrence of the lymphoma.
His pulmonary function varies a bit between normal and a mild obstructive ventilatory defect. His exercise capacity has continued to improve since the BMT, but remains significantly below his pre-morbid state (he was, prior to his cancer, a highly trained endurance athlete).
He is referred for pleuradesis.
His films are below:
His pre-BMT film:

One year later, prior to thoracentesis:

One-day following a 2-liter thoracentesis

Thoughts? How would you proceed?
His pulmonary function varies a bit between normal and a mild obstructive ventilatory defect. His exercise capacity has continued to improve since the BMT, but remains significantly below his pre-morbid state (he was, prior to his cancer, a highly trained endurance athlete).
He is referred for pleuradesis.
His films are below:
His pre-BMT film:

One year later, prior to thoracentesis:

One-day following a 2-liter thoracentesis

Thoughts? How would you proceed?
Monday, October 09, 2006
Change in mental status
45 year old man, presented with a persistant cough that did not go away despite 4 different antibiotic course, some kenalog, some anti-allergy meds, and finally a CXR that showed "Right middle lobe pneumonia"
He was admitted for the persistent cough.
ROS no weight loss, SOB, nightsweats. Just the cough (non productive).
SOCIAL HISTORY: married,self-employed painter. He smokes cigars usually five times a week. He averages six to 12 alcohol beverages per week.
On exam the next day he was alert but confused. His vitals were normal as was his saturation on room air. He did not answer questions. He just looked at his wife and smiled. A Na was 129 when before on admission it was 137. The rest of the labs were unremarkable. LP, EEG and head CT were done but negative. By the trime some of that came back he was already becoming more oriented on his own. The next day he was a/o x 3.
Any feedback before I proceed?
He was admitted for the persistent cough.
ROS no weight loss, SOB, nightsweats. Just the cough (non productive).
SOCIAL HISTORY: married,self-employed painter. He smokes cigars usually five times a week. He averages six to 12 alcohol beverages per week.
On exam the next day he was alert but confused. His vitals were normal as was his saturation on room air. He did not answer questions. He just looked at his wife and smiled. A Na was 129 when before on admission it was 137. The rest of the labs were unremarkable. LP, EEG and head CT were done but negative. By the trime some of that came back he was already becoming more oriented on his own. The next day he was a/o x 3.
Any feedback before I proceed?
Wednesday, October 04, 2006
Dyspnea and a LUL mass
Here's a case from Arenberg:
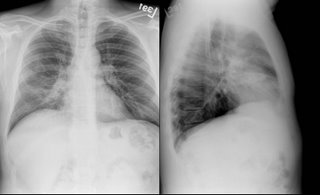
This is 69-year-old lady with coronary artery disease, diastolic congestive heart failure, and dyspnea on exertion. She came to see me because her cardiologist said she has been experiencing increased dyspnea out of proportion to her normal symptoms for ~3 months. Other than a pacemaker over her left chest, her plain chest x-rays were normal
and her pulmonary function tests were mildly restrictive (FVC ~69%), actually improved from her last testing ~ 4 years prior.
I got a VQ scan that was normal, but only on her second visit (when I actually asked) did I learn that she has had 2 birds as house pets for the last 3 years. She further revealed that she has felt unwell going back about 2-1/2 years. One of the birds was in fact sick, and during this time, she fed the bird from mouth to mouth. Yes, I am serious. She was DEAD SET against getting rid of the birds, so I got a CT scan in anticipation of doing a bronch, to prove she had HP.

The CT showed very subtle changes of ground glass, and was actually read as no evidence of ILD, but surprise surprise, she now had a LUL mass that was not seen on the CXR taken 2 months earlier. The radiologist thought it was likely to be inflammatory. What would you do?
I have more images, and some cool pictures to follow, but I’ll hold onto them until people have a chance to comment.
--------------------------
UPDATE:
"...good evidence for chronic HP in the form of a patchy chronic
bronchiolitis that includes occasional multinucleated giant cells of the
sort commonly seen in that condition"
Comments from our pathologist.
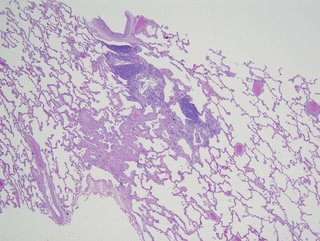
This is 69-year-old lady with coronary artery disease, diastolic congestive heart failure, and dyspnea on exertion. She came to see me because her cardiologist said she has been experiencing increased dyspnea out of proportion to her normal symptoms for ~3 months. Other than a pacemaker over her left chest, her plain chest x-rays were normal
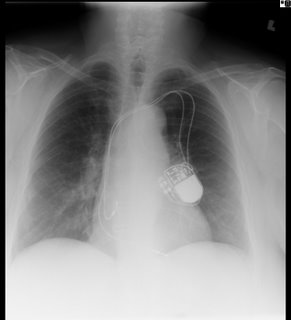
and her pulmonary function tests were mildly restrictive (FVC ~69%), actually improved from her last testing ~ 4 years prior.
I got a VQ scan that was normal, but only on her second visit (when I actually asked) did I learn that she has had 2 birds as house pets for the last 3 years. She further revealed that she has felt unwell going back about 2-1/2 years. One of the birds was in fact sick, and during this time, she fed the bird from mouth to mouth. Yes, I am serious. She was DEAD SET against getting rid of the birds, so I got a CT scan in anticipation of doing a bronch, to prove she had HP.

The CT showed very subtle changes of ground glass, and was actually read as no evidence of ILD, but surprise surprise, she now had a LUL mass that was not seen on the CXR taken 2 months earlier. The radiologist thought it was likely to be inflammatory. What would you do?
I have more images, and some cool pictures to follow, but I’ll hold onto them until people have a chance to comment.
--------------------------
UPDATE:
"...good evidence for chronic HP in the form of a patchy chronic
bronchiolitis that includes occasional multinucleated giant cells of the
sort commonly seen in that condition"
Comments from our pathologist.
Tuesday, October 03, 2006
Varenicline
Have you had the chance to start patients on Chantix yet?
What has your experience with it been thus far? Any good success stories?
What has your experience with it been thus far? Any good success stories?
Friday, September 29, 2006
Sepsis and steroids
IS:
This is not a case presentation, but want to take a poll on what people are doing about steroids and sepsis. Do you administer steroids emperically after initial fluid bolus or do you attempt resuscitation per the 6hr bundle first and then administer steroids if still on pressors or hypotensive?
This is not a case presentation, but want to take a poll on what people are doing about steroids and sepsis. Do you administer steroids emperically after initial fluid bolus or do you attempt resuscitation per the 6hr bundle first and then administer steroids if still on pressors or hypotensive?
Tuesday, September 26, 2006
Follow-up to Anti-GM-CSF
I had posted this question but had no takers so I am posting a suggested answer. The Cleveland Clinic has an (investigational) Anti-GM-CSF autoantibody kit available for primary PAP. Check out this link for more info.
fluid filled lesion
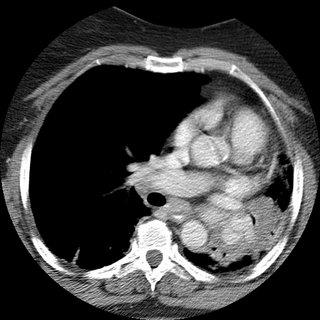
Update on Mass and Infiltrates
I had posted on this 59 y/o woman with a funny presentation: she had had an episode of syncope at home, hit her head and had a skin lac requiring 7 stitches. While being worked up in the ER they found her to be hypotensive and febrile with an abnormal CxR and CT of the chest. She had MSSA in her sputum and a dense lung "mass". I bronch'ed her and got "organizing pneumonia" but no malignancy. She got ABTx and the "mass" went away completely. She did however had persistent smallish alveolar infiltrates seen below:

I re-bronched her focusing on the infiltrates since they had persisted for 3 months after the initial presentation. She had a lot of eosinophilic proteinaceous alveolar material and our pathologists sent the tissue to T. Colby who thought this was PAP.
Would you be satisfied with this Dx on TBBx or would you pursue an OLBx?
How about testing for anti-GM-CSF Antibodies?
She has almost normal lung function, how would you treat her?

I re-bronched her focusing on the infiltrates since they had persisted for 3 months after the initial presentation. She had a lot of eosinophilic proteinaceous alveolar material and our pathologists sent the tissue to T. Colby who thought this was PAP.
Would you be satisfied with this Dx on TBBx or would you pursue an OLBx?
How about testing for anti-GM-CSF Antibodies?
She has almost normal lung function, how would you treat her?
Hemodynamics
A patient intubated and sedated for hypoxia (history of aspiration although CXR negative) had initial swan numbers of: CO 5 L, CI 3.24 PAP 26/16. PCW 8 with cvp of 4. SVR 1362. PVR is 190. AFter fluid boluses with no change in CO, PCW still 8 with a CVP of 6. His SBP has been 116/78 basically unchanged throughout. After fluid blouses he is now about 10 L up with really no change in the above swan readings or bloodpressure. How would you interpret this? Of note a surface echo showed an EF of 25-35%.
Here's his cxr.

Here's his cxr.

Thursday, September 21, 2006
Anti-GM-CSF antibodies
Have you been checkin anti-GM-CSF antibodies for evaluation of suspected PAP? If so, is there a commercially available ELISA or have you been sending those to the Cleveland Clinic?
Monday, September 18, 2006
Follow-up to Pulmonary-thyroid
This is the patient with the hot pulmonary nodule and lung mass.
We decided to start with the thyroid and a bronch. The thyroid mass (it was not cystic on CT) was a follicular carcinoma with local invasion. No lymphnodes and the other lobe was clean.
The bronch was non-diagnostic and radiology felt the mass was too low and there was too much lung in its way for a good CT-guided needle.
She went to see our CT surgeons and we figured out why the bronch was non-diagnostic: it was not a lung mass but a diaphragmatic mass. It was an aneuploid adenomatoid tumor still not clearly characterized. Incidentally, there was a second focus of this same adenomatoid tumor in the superior segment of that LLL, which had not been seen on CT or PET (at ~7mm).
What do you think?
We decided to start with the thyroid and a bronch. The thyroid mass (it was not cystic on CT) was a follicular carcinoma with local invasion. No lymphnodes and the other lobe was clean.
The bronch was non-diagnostic and radiology felt the mass was too low and there was too much lung in its way for a good CT-guided needle.
She went to see our CT surgeons and we figured out why the bronch was non-diagnostic: it was not a lung mass but a diaphragmatic mass. It was an aneuploid adenomatoid tumor still not clearly characterized. Incidentally, there was a second focus of this same adenomatoid tumor in the superior segment of that LLL, which had not been seen on CT or PET (at ~7mm).
What do you think?
Friday, September 15, 2006
Wednesday, September 13, 2006
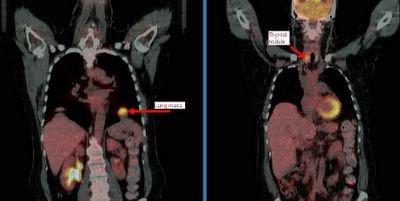
The pulmonary-thyroid connection

This patient came to me pre-worked up so I will show all the data she had had thus far. This is a 65 y/o woman with no TOB Hx, normal PFTs who had a persistent cough. She had an abnormal CxR (see above) and here PCP ordered a CT and then a PET-CT and she was sent to us.
Her PET scan showed two very FDG-avid lesions. A L basilar lung lesion and a R thyroid nodule with no other abnormal uptake. She is euthyroid clinically and by TFTs.
Do you think the lesion are related?
Would you biopsy one, the other, both?
Tuesday, September 12, 2006
LUL lesion, still undiagnosed
70 year old woman with COPD FEV1 34% predicted, but she is well compensated and on no supplemental oxygen (91% on RA). A LUL lesion was noted (see below) and workup included 2 bronchs (one with ultrasound-guided) and 1 CT-guided biopsy. All were negative for malignant cells. BAL was not done but Tbbx showed Atypical lymphoid cell with acute inflammation and Filamentous bacteria. BAL was not sent so we don't have micro ID (the bacteria was identified by path).
Cancer is obviously still number one on the list, but I dont think she's a surgical candidate and in terms of treating with chemo, we still dont have a tissue diagnosis. On the other hand, the filamentous bacteria finding is interesting. What is your impression and what would you all do next? Thanks.
Cancer is obviously still number one on the list, but I dont think she's a surgical candidate and in terms of treating with chemo, we still dont have a tissue diagnosis. On the other hand, the filamentous bacteria finding is interesting. What is your impression and what would you all do next? Thanks.
Monday, September 11, 2006
Bloody effusion
57 y/o man former smoker, presented with pleuritic CP and found to have left loculated effusion. No constitutional sx. no wt loss, fever, chills, cough. Tap 2 weeks later showed it to be bloody, with 57 WBC, 49% PMN and 49% lymphocytes. He is currently asymptomatic.
The effusion was AFB - times 1. The micro and cytology was negatrive. Dopplers of legs negative and V/Q was intermediate or indeterminate (cant remember) and PE-protocol CT was read as negative.
His Pmhx not remarkable except for 2 previous pneumonias. Last was in march and was on the right side. There was a small parapneumonic effusion which has since resolved.
No history of trauma except moving his furniture 1 day before the pleuritic CP, but he did not hit anything per se. No Fmhx of thrmbosis and in fact his Wells criteria is zero.
What would you all do next?
The effusion was AFB - times 1. The micro and cytology was negatrive. Dopplers of legs negative and V/Q was intermediate or indeterminate (cant remember) and PE-protocol CT was read as negative.
His Pmhx not remarkable except for 2 previous pneumonias. Last was in march and was on the right side. There was a small parapneumonic effusion which has since resolved.
No history of trauma except moving his furniture 1 day before the pleuritic CP, but he did not hit anything per se. No Fmhx of thrmbosis and in fact his Wells criteria is zero.
What would you all do next?
Thursday, September 07, 2006
Advice on further workup for this lung cancer.
59 year old ex-smoker with FEV1 1.17 liters (47% predicted) who has a left upper lobe lesion:
He also has some enlarged nodes (red circles):
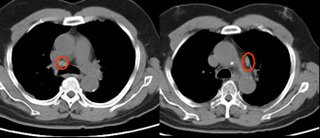
The PET showed intense uptake of the LUL lesion and "mild hypermetabolic activity in the right hilar and pericarinal regions corresponding to nonenlarged lymph nodes on CT. This is of uncertain clinical significance. No other foci of abnormal hypermetabolic activity are identified.":
However, because of the enlarged nodes and the equivocal uptake on PET , I elected to sample them anyway;
The results showed no malignancy from the fine needle aspirate (but there were lymphocytes indicating that the node was sampled.
Not surprisingly, biopsy of the peripheral lesion in the LUL lesion was indeed cancer - adenocarcinoma.
Would you call this cancer a stage I (tumor was 2.4 x 1.4 cm) and proceed to surgery?
He also has some enlarged nodes (red circles):
The PET showed intense uptake of the LUL lesion and "mild hypermetabolic activity in the right hilar and pericarinal regions corresponding to nonenlarged lymph nodes on CT. This is of uncertain clinical significance. No other foci of abnormal hypermetabolic activity are identified.":
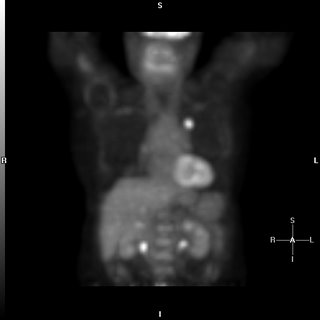
However, because of the enlarged nodes and the equivocal uptake on PET , I elected to sample them anyway;
The results showed no malignancy from the fine needle aspirate (but there were lymphocytes indicating that the node was sampled.
Not surprisingly, biopsy of the peripheral lesion in the LUL lesion was indeed cancer - adenocarcinoma.
Would you call this cancer a stage I (tumor was 2.4 x 1.4 cm) and proceed to surgery?
Wednesday, September 06, 2006
Multiple pulmonary nodules
The patient is a 69-year-old African-American woman who came to pulmonary clinic for multiple pulmonary nodules that were picked up in the course of abdominal CT for workup for abdominal pain with increased LFTs (which have since normalized). She has a history of hypertension, diabetes, peripheral vascular disease, and hyperlipidemia. She is a nonsmoker. No fever chills cough SOB, diaphoresis or constitutional symptoms.
Exam: A pleasant woman in no acute distress. WT of 197, BP 185/83, P is 65, R 18, O2 sat is 97% on room air. Trachea midline. No lymphadenopathy and no supraclavicular adenopathy. No thyromegaly. Lungs: Clear to auscultation. No wheezing, rales, or rhonchi. No dullness to percussion. No egophony, symmetric chest wall on inspiration. Heart: Regular rate. S1, S2. Abdomen: Positive bowel sounds. No masses. No liver edge felt. No clubbing, cyanosis, or edema.
Data:
PFT's: FEV1/FVC 81, FEV1 76% predicted, FVC 73% predicted.
CBC with hemoglobin of 10.3, MCV of 94.6. Plts normal. Lytes-7 normal. ANA and rheumatoid factor negative
These nodules are all non-calcified. The largest is 8 mm. There is interval growth of left lower lobe nodule and right apical nodule compared to a CT 6 months prior. The subcarinal soft tissue is "prominent" but ambiguous whether it's enlarged.
On abd CT, the spleen, pancreas, kidney, gallbladder and adrenals are unremarkable.
2 calcified hepatic granulomas are seen.
Any thoughts on workup or management?
.
Exam: A pleasant woman in no acute distress. WT of 197, BP 185/83, P is 65, R 18, O2 sat is 97% on room air. Trachea midline. No lymphadenopathy and no supraclavicular adenopathy. No thyromegaly. Lungs: Clear to auscultation. No wheezing, rales, or rhonchi. No dullness to percussion. No egophony, symmetric chest wall on inspiration. Heart: Regular rate. S1, S2. Abdomen: Positive bowel sounds. No masses. No liver edge felt. No clubbing, cyanosis, or edema.
Data:
PFT's: FEV1/FVC 81, FEV1 76% predicted, FVC 73% predicted.
CBC with hemoglobin of 10.3, MCV of 94.6. Plts normal. Lytes-7 normal. ANA and rheumatoid factor negative
These nodules are all non-calcified. The largest is 8 mm. There is interval growth of left lower lobe nodule and right apical nodule compared to a CT 6 months prior. The subcarinal soft tissue is "prominent" but ambiguous whether it's enlarged.
On abd CT, the spleen, pancreas, kidney, gallbladder and adrenals are unremarkable.
2 calcified hepatic granulomas are seen.
Any thoughts on workup or management?
.
Tuesday, September 05, 2006
Pulmonologist with high IgE
At ATS there was a stand on a rapid IgE testing system on capillary blood and some of us had it done just to check out the system.
One of us (with Hx of rhinitis but noasthma) had the results come back at an IgE level of 900 (their upper limit was 136).
Would you investigate it any further (CBC with diff, etc.) ?
One of us (with Hx of rhinitis but noasthma) had the results come back at an IgE level of 900 (their upper limit was 136).
Would you investigate it any further (CBC with diff, etc.) ?
Thursday, August 31, 2006
Benign uterine fibroids and pleural effusion
This is an outside submission for a question correlating a pleural effusion and Gyn disease:
Patient with a right pleural effusion, more than 1500 ml tapped. 2nd tap: more than 1700 ml tapped 6 days later. Contrast CT revealed pelvic fibroids.
Effusion results protein, probably assoc. w/ RBC.5 to 11 months prior, sonograms, contrast MRI revealed uterine fibroids 8 to 10 mm in size, stable in size over 6 months. Uterine scrape (not complete D and C) test benign. No indications of ovarian cysts, etc. Hysterectomy not chosen due to stable fibroid size and results of uterine scrape.Heavy coughing for 9 mos. Chronic post-nasal drip for 23 mos.
Allergy tests reveal slight allergy to a few local plants.
Chest xray showed: Pleural effusion right side.
Latest contrast CT pelvic fibroid.Previous ultrasound and contract MRI showed uterine fibroids stable after approx 6 mos.
Effusion samples from 2 taps have no cytology assoc. w/cancer, no pancreatitis, tb/fungus results not yet available. Unremarkable except for protein.
2D echo unremarkable.
Any suggestions on this reaccumulating effusion?
Patient with a right pleural effusion, more than 1500 ml tapped. 2nd tap: more than 1700 ml tapped 6 days later. Contrast CT revealed pelvic fibroids.
Effusion results protein, probably assoc. w/ RBC.5 to 11 months prior, sonograms, contrast MRI revealed uterine fibroids 8 to 10 mm in size, stable in size over 6 months. Uterine scrape (not complete D and C) test benign. No indications of ovarian cysts, etc. Hysterectomy not chosen due to stable fibroid size and results of uterine scrape.Heavy coughing for 9 mos. Chronic post-nasal drip for 23 mos.
Allergy tests reveal slight allergy to a few local plants.
Chest xray showed: Pleural effusion right side.
Latest contrast CT pelvic fibroid.Previous ultrasound and contract MRI showed uterine fibroids stable after approx 6 mos.
Effusion samples from 2 taps have no cytology assoc. w/cancer, no pancreatitis, tb/fungus results not yet available. Unremarkable except for protein.
2D echo unremarkable.
Any suggestions on this reaccumulating effusion?
Wednesday, August 30, 2006
Diagnosis and staging of lung cancer
Anonymous asks, If a patient, on chest CT, has a mass invading the hilum and mediastinum and there is also a pleural effusion, would you be able to simply do a thoracentesis for cytology and forego the bronch?
My take is that a bronchoscopy would not be neccessary, as a positive effusion will both diagnose and stage it as a T4. What do you think?
My take is that a bronchoscopy would not be neccessary, as a positive effusion will both diagnose and stage it as a T4. What do you think?
Monday, August 28, 2006
35 year old with cough, chills
35 year old without PMhx except a MVA 5 years ago, anxiety and depression. Now with chills and subjective fever and weight loss for the past few months. Meds: Paxil. Fhx: brother died of liver failure, patient does not know etiology. SH denies IVDA. 2 PPD x 20 years. Quit 5 yrs ago. HIV negative. Exam Afebrile. VSS. Some decr breath sounds upper lung zones b/l. WBC 11.

What would you do next?

What would you do next?
Alpha-1 AT
So, I saw a patient last week for Alpha-1 AT deficiency. Phenotypically, she has the disease--lower lobe emphysema, severe obstructive disease (FEV1 of 1.0 L which improved to 1.35 while on augmentation therapy with Prolastin). She has a family history of the disease and is a non-smoker (with substantial second-hand exposure). Her measured enzyme level, prior to the start of weekly Prolastin, was 31 mg/dl (lab range for normal is 100-190 mg/dl).
So, the interesting thing is that she (and her family members with the disease) has an M-Z genotype, which should be a "normal" phenotype without disease. The genotype was confirmed with separate studies, as was her son's genotype.
Anyone seen this before? Any comments?
So, the interesting thing is that she (and her family members with the disease) has an M-Z genotype, which should be a "normal" phenotype without disease. The genotype was confirmed with separate studies, as was her son's genotype.
Anyone seen this before? Any comments?
Thursday, August 24, 2006
Prune-belly
I have just seen a 26 y/o patient in the office for recurrent respiratory tract infections. He has a Hx of prune-belly syndrome (poor abdominal muscle development with severe urinary tract abnormalities) and has been on HD after a failed renal Txp.
These patients tend to have a restrictive physiology because of the oligohydramnios and sometimes even have hypoplastic lung. Indeed his TLC is ~66%. His Cxr is pretty unremarkable but he also has an associated obstructive defect: FEV1 is ~36% witha ratio of<70%. Has anybody seen this condition (or similar ones) be associated with asthma/reactive airways disease?
These patients tend to have a restrictive physiology because of the oligohydramnios and sometimes even have hypoplastic lung. Indeed his TLC is ~66%. His Cxr is pretty unremarkable but he also has an associated obstructive defect: FEV1 is ~36% witha ratio of<70%. Has anybody seen this condition (or similar ones) be associated with asthma/reactive airways disease?
Tuesday, August 22, 2006
CPET
What do you think of this CPET data?
61 y/o obese woman (BMI: 37.3), S/P remote CABG with patent grafts and normal LVEF on recent angiography with persistent DOE. Very remote smoking Hx with only a mild restrictive defect (FVC~70% with FEV1/FVC>80), normal DLCO and normal HRCT. Negative methacholine challenge.
DATA (predicted values and/or percentages):
VO2max (ml/kg/min): 14.4 (25.4/56%)
AT: 0.749 (>0.698) - 43% predicted VO2max (>40%)
Max HR 73% predicted with still good reserve: 44. O2 pulse 11.5 (8.4)
VE max: 50.7 (65.9 / 77%)
Vt: 1.28 (0.563)
Respiratory rate: 36 (<50)
Breathing reserve: 2% (20-40%)
Vd/Vt at rest: 0.51 (0.30)
Vd/Vt at peak: 0.26 (0.18)
RQ: 0.93 (1.1-1.3)
No desat.
FVC at peak declined by 19% and FEV1 at peak did not change.
61 y/o obese woman (BMI: 37.3), S/P remote CABG with patent grafts and normal LVEF on recent angiography with persistent DOE. Very remote smoking Hx with only a mild restrictive defect (FVC~70% with FEV1/FVC>80), normal DLCO and normal HRCT. Negative methacholine challenge.
DATA (predicted values and/or percentages):
VO2max (ml/kg/min): 14.4 (25.4/56%)
AT: 0.749 (>0.698) - 43% predicted VO2max (>40%)
Max HR 73% predicted with still good reserve: 44. O2 pulse 11.5 (8.4)
VE max: 50.7 (65.9 / 77%)
Vt: 1.28 (0.563)
Respiratory rate: 36 (<50)
Breathing reserve: 2% (20-40%)
Vd/Vt at rest: 0.51 (0.30)
Vd/Vt at peak: 0.26 (0.18)
RQ: 0.93 (1.1-1.3)
No desat.
FVC at peak declined by 19% and FEV1 at peak did not change.
Monday, August 21, 2006
Anemia
This is more of a critical care than pulmonary question. It came up today in discussion with renal...
The gold satndard for iron-def. anemia has been staining the bone marrow for iron stores. Nobody does that much anymore as first test since ferritin has such a good correlation with iron stores. The discussion was whether you can have iron-deficiency anemia with good normal ferritin (not normal-low, low-normal, borderline, etc.). Even though ferritin is an acute phase reactant and may mak a borderline ferritin level seem normal it shouldn't push it to the mid-high range. (ferritin will roughly triple as an acute phase marker, Ann Rheum Dis 1986 Jul;45(7):596-602)
Do you look at the iron/iron sat or do you trust the ferritin?
The gold satndard for iron-def. anemia has been staining the bone marrow for iron stores. Nobody does that much anymore as first test since ferritin has such a good correlation with iron stores. The discussion was whether you can have iron-deficiency anemia with good normal ferritin (not normal-low, low-normal, borderline, etc.). Even though ferritin is an acute phase reactant and may mak a borderline ferritin level seem normal it shouldn't push it to the mid-high range. (ferritin will roughly triple as an acute phase marker, Ann Rheum Dis 1986 Jul;45(7):596-602)
Do you look at the iron/iron sat or do you trust the ferritin?
Thursday, August 17, 2006
Failure to wean
This is a 44 year old man with DM, s/p renal transplant several years ago. He has the other associated micro- and macro- vascular problems associated with DM, including severe PVOD and a non-healing, chronic LE cellulitis for which a BKA has been recommended (but refused--he is on chronic supressive antibiotics). His immunosupression includes cyclosporine and prednisone.
He was admitted to the ICU with hypoxemic respiratory failure requiring intubation for what turned out to be herpes pneumonitis, and was treated with a 21 day course of acyclovir. Over this course, he was easily ventilated and oxygenated with progressively improving respiratory parameters. On two occasions, his weaning parameters were excellent, and he easily tolerated minimal ventilatory support (PS-5/PEEP 5) for 2 hours. Each time, he required re-intubation for respiratory distress several hours after extubation.
Here's some representative cuts from a CT scan done about 10 days into his hospital course.

He was admitted to the ICU with hypoxemic respiratory failure requiring intubation for what turned out to be herpes pneumonitis, and was treated with a 21 day course of acyclovir. Over this course, he was easily ventilated and oxygenated with progressively improving respiratory parameters. On two occasions, his weaning parameters were excellent, and he easily tolerated minimal ventilatory support (PS-5/PEEP 5) for 2 hours. Each time, he required re-intubation for respiratory distress several hours after extubation.
Here's some representative cuts from a CT scan done about 10 days into his hospital course.

Tuesday, August 15, 2006
PET and staging
I saw this patient in follow-up today.
This is an 82 y/o woman with no smoking history but decades of second-hand smoke (her husband died of lung dz). She had a dry cough and a CT scan was done. She has the large LUL mass seen on the CT cut (on an outside CT with contrast, the mass seems to invade the PA). I did a bronch and the mass is a non-small cell Ca. Unfortunately, the hilar TBNA were non-diagnostic. Her PET scan shows marked uptake by the mas, ipsi- and contralateral hilar nodes and pre-tracheal nodes.
With the PA involvement (on CT) and the PET results would you be satisfied in calling it a IIIB or would you do a mediastinoscopy to confirm either/both with tissue?

This is an 82 y/o woman with no smoking history but decades of second-hand smoke (her husband died of lung dz). She had a dry cough and a CT scan was done. She has the large LUL mass seen on the CT cut (on an outside CT with contrast, the mass seems to invade the PA). I did a bronch and the mass is a non-small cell Ca. Unfortunately, the hilar TBNA were non-diagnostic. Her PET scan shows marked uptake by the mas, ipsi- and contralateral hilar nodes and pre-tracheal nodes.
With the PA involvement (on CT) and the PET results would you be satisfied in calling it a IIIB or would you do a mediastinoscopy to confirm either/both with tissue?

Subscribe to:
Posts (Atom)