I had seen this 76 y/o man about 18 months ago for "abnormal CxR". He had "dry" crackles, a mild restrictive defect (FVC, FEV1 and TLC all around 70%) and a HRCT very typical for IPF. I had discussed prognosis and treatment options and suggested a referral to the nearby University center for possible enrollment in a trial. He felt fine and declined the referral. He continued to see his PCP but had cancelled his follow-up with me. He then came back because of worsening dyspnea and hypoxemia (he is now on 3L/min O2) and his FVC is down to 45%.
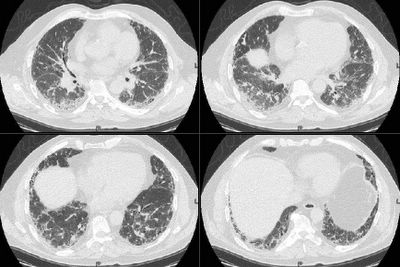
I have attached a recent CT image below. He is obviously not a transplant candidate and he does not want to enroll in clinical trials. What medical therapy (if any) would you offer him?
Thursday, January 12, 2006
Subscribe to:
Post Comments (Atom)
3 comments - CLICK HERE to read & add your own!:
The current "standard of care" (unfortunately) is Pred/Azathioprine + NAC. I say unfortunately, because one interpretation of the recent study (which contained NO PLACEBO ARM), is that the addition of NAC improves outcomes compared the AZA/Pred alone. The problem is that there have never been data showing that AZA/Pred is beneficial, and there are data that AZA/Pred may do harm. Additionally, the "benefit" from the addition of NAC is mild, at best.
So, the best option is to get the patient into a study somewhere. The next "best option" would be AZA/Pred/NAC if he can tolerate it. There are no data looking at NAC alone vs placebo or versus AZA/Pred.
Of course, we all know some who would argue that this patient should not be treated. This is where I'd have a very long discussion with the patient about the risks and benefits (or lack thereof) of therapy...
I recommended trial enrollment but he was not interested. When we discussed possible therapies I tried to emphasize the lack of positive data and some of the pros- and cons-... He was started on AZA/Pred and felt better (maybe just a bit of the steroid effect). He has been on that for 3 months with stable severe restriction and I will try adding NAC on his next visit.
The NEJM study showed improvement just in physiologic parameters. Changes in dyspnea and in extent of fibrosis on CT were similar in the two groups, and no significant difference was found in mortality rates. So, no improvement in hard outcomes. I would take this as a negative study.
Post a Commenttest post a comment