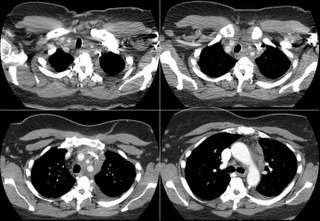
A CT showed a big ol' mass:
 The biopsy is quite interesting. Here's the report: The biopsy contains no normal tissue. All sections contain confluent non-necrotizing granulomas with patchy associated lymphocytic infiltrate. Per the accompanying report, special stains are reported to be negative for fungus and acid fast bacteria.
The biopsy is quite interesting. Here's the report: The biopsy contains no normal tissue. All sections contain confluent non-necrotizing granulomas with patchy associated lymphocytic infiltrate. Per the accompanying report, special stains are reported to be negative for fungus and acid fast bacteria.What are your thoughts about what's going on, and how would you proceed next? There are no "right" answers yet as the workup is ongoing. All comments are helpful.
3 comments - CLICK HERE to read & add your own!:
That pathology is most notable for the non-caseating granulomas. This would not be consistent with fibrosing mediastinitis, which Keena mentioned in his previous post and which was a great suggestion.
Was the biopsy of this done by mediastinoscopy, or was it a 19g Wang. If it was a Wang, then I wouldn't rule out lympoma.
Otherwise, this pathology and presentation are consistent with Sarcoidosis. Although rare, there are several reports of Sarcoidosis presenting with/associated with chylothorax-usually due to massive lymphadenopathy compressing the thoracic duct.
See: Soskel, NT and Sharma, OP
Curr Opin Pulm Med. 2000 Sep;6(5):455-68.
The biopsy was via fine needle aspiration under bronchoscopy from an outside hospital. I do not know the needle gauge for that. The patient is going to be bronched again and with TBBx.
Fungal serologies and a PPD skin test were negative.
I think you'll eventually need to do a surgical biopsy to get diagnostic tissue and definitively rule out lymphoma.
Post a Commenttest post a comment