58-year-old lady known to have multiple medical problems including rheumatoid arthritis diagnosed about 14 years ago. She was evaluated for a possibility of recurrence of kidney stones and kidney problems and had CT of the abdomen. On the lung cuts of that CT scan, there was a lung nodule and that was further investigated by a dedicated CT of the thorax. The patient was referred to us for further evaluation and management of the small nodule. The patient denies having any cough on a regular basis. No history of hemoptysis. She has shortness of breath upon heavy exertion and can climb two flights without problems. No fever or chills.
MEDICATIONS: The patient is currently on Enbrel injection twice a week. She is also on Levoxyl 0.125 mg p.o. once per day, Protonix 40 mg p.o. once per day, and multivitamins. She received methotrexate in the past for 1 year, and stopped it secondary to LFT disturbance. Last methotrexate dose 6 years ago.
SOCIAL HISTORY: The patient smoked in the past for 30 to 35 years and at that she smoked one-and-a-half pack per day. She quit smoking 11 years ago. She denies drinking or using any illicit drugs. She had multiple jobs in the past and that included working for a trucking
company as a dispatcher and also a supervisor. She also currently is doing flower arrangements and sewing crochet.
PFT:
FVC 2.67 (72)
FEV1 2.06 (71) with 6% post-bronch change
FEV1/FVC 77.2% (98% preicted)
TLC Liters 3.80 (69%)
VC Liters 2.67 (72)
FRC N2 Liters (1.77) 3.12 (57)
ERV Liters (0.50) 1.02 (49)
RV Liters (1.13) 2.09 (54)
RV/TLC 29.8 (78%)
Diffusion
Hb: CO Hb:
DLCO mL/mmHg/min 20.3 (88%)
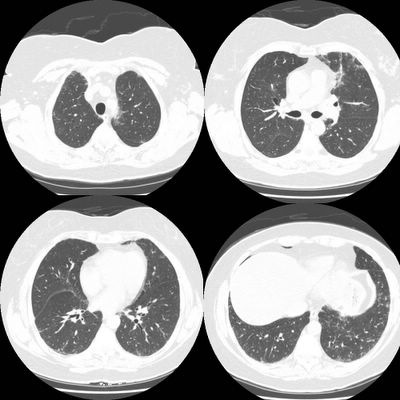
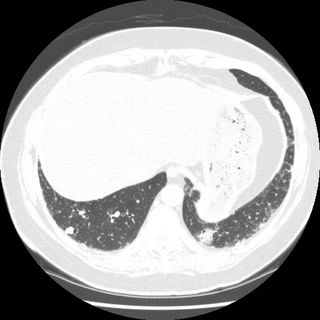
Imaging studies: High resolution CT thorax:
There is subpleural reticular change, mostly in the lung bases, with lesser amounts in the upper lobes. There is some ground-glass and each upper lobe also an suggestion of minimal honeycombing in the left upper lobe. The changes in the lower lobes have progressed since the prior study done 3 months earlier Representative slices, from apex to base are shown below.
There was a concern about ILD related to the rheumatoid. Bronchoscopy was done with BAL showing:
CELL CT./DIFF, FLUID
RBC 31 /cu mm
WBC 224 /cu mm
NEUTROPHILS 31%, LYMPHOCYTES 36 % MONOCYTES 10%, EOSINOPHIL 21 %
FUNGAL CULT: No yeast or hyphal elements seen
AFB SMEAR No acid fast bacilli seen
Transbronchial biopsies were not done (patient coughing).
Summary: 58 y.o lady with severe rheumatoid arthritis on Remicade, with restrictive ventilatory defect and normal diffusion, with mild honeycombing/ early fibrotic changes that seem to be progressing over 3 months, with eosinophilia and lymphocytosis on the BAL. what is the next step?
6 comments - CLICK HERE to read & add your own!:
Do you think the eos count of 21% suggests an etiology other than RA-ILD?
I think the 21% eosinophilia is a distractor in this case. That degree of eosinophilia is consistent with collagen-vascular associated ILD, which is what I think this is.
She has restriction, sub-pleural interstitial changes, and honeycombing. That's UIP due to RA. Unlike scleroderma, the increased neutrophila in RA doesn't really portend an improved response, but give that and the ground glass, I would still try some steroids or another immunosupressant.
BOOP! This had to be done.
Mendez's diff diagnosis is good, but have you thought about an allergic reaction in the lung with that quantity of eos. Especially to the Enbrel or methotrexate. Any peripheral eosinophilia? You may want to change her agent again as she seems to be progressing despite (or perhaps because of) Enbrel.
Any travel to foreign countries or other risks for parasitic disease?
Are their any micronodules in the upper lobe c/w hypersensitivity pneumonitis. Can we see the images? Transbronchial bx may be useful if there are poorly formed granulomas.
Also, I think (and please correct me if I am wrong) the diff is pretty normal for a patient with ILD. As Mike said, there is no data in patients with RA, but BAL is helpful in patients with SLE. I cannot find the reference (if anyone can, I would be obliged), but neutrophilia marks disease activity.
Thank you all for the responses. At this time, We decided to follow her at 3 months interval with PFT and HRCT, given her minimal respiratory symptoms, and stable PFT/normal DLCO.
So what is your working diagnosis?
The working dx is radiographic changes consistent with RA-ILD. Treatment (above the current regiment of enbrel) was discussed and the decision was to follow given the lack of symptomatology and the stable PFT's.
Repeat PFT's and HRCT will be done in 3 months. A pulse of steroids will be given at that time if any of the following decline: pft's, HRCT progression, or development of dyspnea.
Post a Commenttest post a comment