We were consulted on this pleasant 58-year-old white male with known coronary artery disease. He was last admitted 3 months ago with a inferior lateral wall myocardial infarction. He is status post angioplasty. He has a history of chronic obstructive pulmonary disease. He had been doing fairly well andhad gone back to work as an electrician however, over the last five days he developed increasing lethargy, chills and felt feverish with a dry nonproductive cough and worsening dyspnea.
PMHx: Ventricular tachycardia, S/P AICD/PM. CAD, S/P inferior lateral myocardial infarction and previous EF~45%. He is status post stenting of the OM/circumflex. Chronic obstructive pulmonary disease. Dyslipidemia.
Current meds: Lovenox, Albuterol and Atrovent, Levofloxacin, Aspirin and Amiodarone.
FHx: Noncontributory
SHx: Heavy cigarette smoker, he quit 3 months ago. He has been drinking several beers daily. He works as an electrician. He lives alone and his wife died last year.
ROS non-contributory.
On exam he was tachypneic to 36 with an O2Sat of 90% on BiPAP with 100% FiO2. BP and HR were stable. His lungs had very faint crackles and no wheezing or ronchi.
ABG was: 7.43/CO2: 37/ O2: 58 on 100% FM.
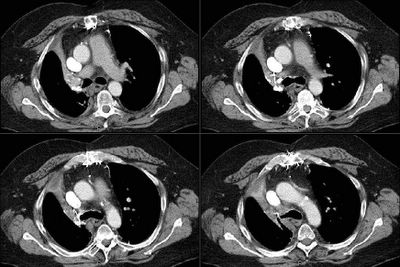
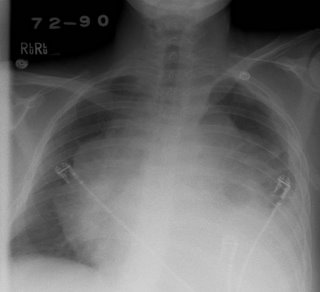
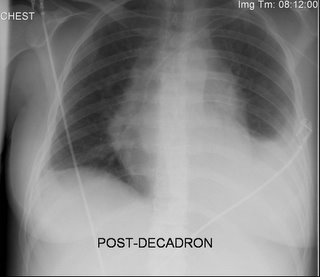
His CxR and CT are posted below.
What would you do next?



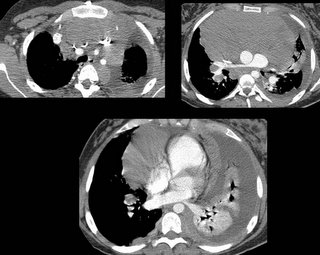

 A CT scan was performed, confirming a 3 cm vertically oriented cylindrical lesion.
A CT scan was performed, confirming a 3 cm vertically oriented cylindrical lesion.