This is a 54 y/o man with a 2-pack day TOB habit who had been referred to us for atypical chest pain. He complained of intermittent chest tightness and had had a negative cardiac w/up (normal SPECT-stress, normal EF, etc.). We identified a mild to moderate obstructive ventilatory deffect (normal FVC and FEV1 that fluctuated between high 50s to 70%) and started him on bronchodilators and continued to counsel him about smoking. He had a CxR with a RUL bulla and some L apical scarring. In the course of his follow-up however, we performed a repeat CxR which revealed a new LUL lesion:
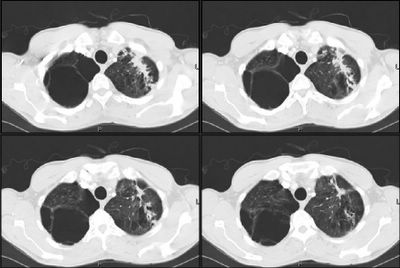
He had some cough at the time so he was given a course of ABTx and followed closely and there was no improvement in the lesion after 4 weeks. A CT scan was obtained and revealed a soft tissue mass associated with some scarring:
A bronch was done and was non-diagnostic and the mass remained unchanged on CxR.
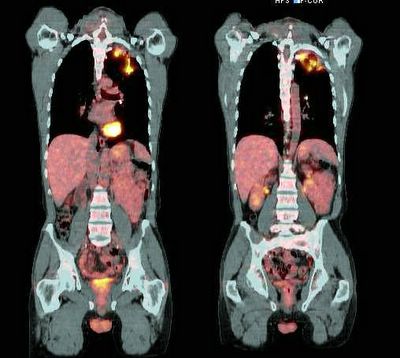
A PET-CT was then performed and revealed intense uptake on the area (SUV ~5.7 about 6 weeks after he had completed the course of ABTx) :
What would you do next?
Subscribe to:
Post Comments (Atom)

2 comments - CLICK HERE to read & add your own!:
That is a pretty high SUV 6 weeks after completion of a course of antibiotics.
Do you have a radiograph showing a normal LUL? If so, what is the time course of its development?
Would he physiologically tolerate a LUL lobectomy?
Depending on the time course of the lesion, I think I would be inclined to ask the surgeon to take it out.
His previous CxRays (not on the computer) did not show that lesion and they were about 12 months old. He does have an 86-pack year of TOB but his lung function would tolerate a LULobectomy...
Post a Commenttest post a comment