We were consulted on this pleasant 58-year-old white male with known coronary artery disease. He was last admitted 3 months ago with a inferior lateral wall myocardial infarction. He is status post angioplasty. He has a history of chronic obstructive pulmonary disease. He had been doing fairly well andhad gone back to work as an electrician however, over the last five days he developed increasing lethargy, chills and felt feverish with a dry nonproductive cough and worsening dyspnea.
PMHx: Ventricular tachycardia, S/P AICD/PM. CAD, S/P inferior lateral myocardial infarction and previous EF~45%. He is status post stenting of the OM/circumflex. Chronic obstructive pulmonary disease. Dyslipidemia.
Current meds: Lovenox, Albuterol and Atrovent, Levofloxacin, Aspirin and Amiodarone.
FHx: Noncontributory
SHx: Heavy cigarette smoker, he quit 3 months ago. He has been drinking several beers daily. He works as an electrician. He lives alone and his wife died last year.
ROS non-contributory.
On exam he was tachypneic to 36 with an O2Sat of 90% on BiPAP with 100% FiO2. BP and HR were stable. His lungs had very faint crackles and no wheezing or ronchi.
ABG was: 7.43/CO2: 37/ O2: 58 on 100% FM.
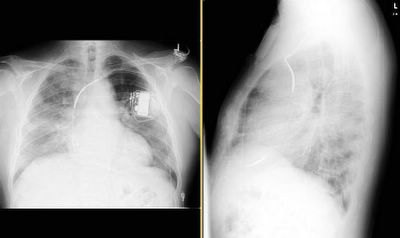
His CxR and CT are posted below.
What would you do next?
Subscribe to:
Post Comments (Atom)


7 comments - CLICK HERE to read & add your own!:
DC amiodarone. If mediastinal windows demonstrate increased attenuation (>40 HU) of the lung parenchyma and of the liver because of iodinated compound of amiodarone, I would also start systemic steroids.
Good observations! He actually had not been on the amio but for a few weeks. He was stil on the "PO loading dose" of 400 mg/day. Good comment on the attenuation. However, the infiltrates were around fat density (-50 to -100s) and not quite as dense.
Besides stopping the amio, would you do anything else at this point?
Oops, I posted my comment at the same time as Mendez. I will give some more time and then post some data on the bronch results.
Of course, amiodarone toxicity is a diagnosis of exclusion. Given that not much information given on other possibilities such as infection or CHF, I assume those are unlikely. Pt is already on BiPAP with 100% FiO2. So, bronch can not be done without intubation. In a real world setting, I would check BNP and treat as CHF with diuretics to avoid intubation together with antibiotics if infection is also a concern.
The use of a BNP in respiratory failure is only helpful for its negative predictive value. In other words, a BNP of < 360 is good for ruling out a cardiac source. However, if it is > 360, all bets are off.
Maisel A. Circulation 2002; 105:2328-31
This test was never meant to be used in the critical care setting with the cutoff of 100... that was an ER study in patients with normal creatinines.
It depends on what cut-off you use. My understanding of BNP is, higher the number, more specific for acute LV dysfunction. Some types of pulmonary disease, such as cor pulmonale, lung cancer, and pulmonary embolism, have elevated BNP levels, but these are not usually elevated to the same extent as in patients with acute LV dysfunction. I agree that if you use a cut-off of somewhere between 100 to 1000, BNP levels can be non-specific, but if a BNP level is sky-high, that can still support the diagnosis of acute LV dysfunction even in the critical care setting.
Start po steroids once any support for amio. toxicity. Pt. can die due to delay with hope of spontaneous resolution. Cover with antibiotics while waiting for results to r/o infection.
Post a Commenttest post a comment