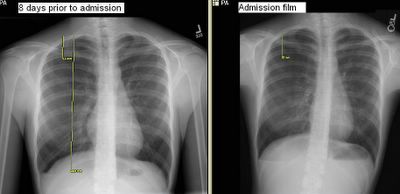
I am not sure if the CxR will show up well. This is a healthy, active, non-smoker 18-y/o woman seen by her pediatrician for mild dyspnea and R chest discomfort. She had the CxR on the left with a spontaneous PTx and he decided to wait and follow it up. She had a repeat CxR 4 days later (not shown) with an unchanged PTx. We were called 4 days later by radiology about the persistent PTx on the film on the right. She is very stable. Her Hx is otherwise really unremarkable except for her cousin having had a recurrent PTx requiring a VATS.
What would you do next?
Would you have waited those eight days just "watching" it?
How do you preferentially handle these pneumothoraces (i.e. Cook cath, Thoravent, chest tubes)?
5 comments - CLICK HERE to read & add your own!:
I cannot see the PTX on the film- monitor does not have great resolution.
I agree with your plan and follow up.
The senior guys in my practice have stories of patients with 100% PTX that they have watched and all resolve without intervention.
As long as she does not worsen from her symptoms, I would probably get a CXR every 1-2 weeks in order to confirm resolution. An 18 year old female will probably want to minimize scarring on her chest (even from a VATS) if it can be avoided.
Alternatively, you could do a thoracentesis to evacuate the air. I did one about 2 months ago with good success (female, 25-ish, and no other medical probs).
If she resolves and gets a 2nd one, she buys a VATS.
I also am having a hard time viewing the CXR. If the PTX is >20% a thoracic surgery consult should be obtained. A PTX that is >20-30% should be treated with a chest tube that is connected to a Pleurevac and watched as an inpatient (A pigtail cath can be connected to a pleurevac to minimize scar size). Once there is no detectable "airleak" and the lung is fully expanded on CXR the chest tube can be removed. If the patient is a pilot or scuba diver VATS should be considered otherwise no surgical intervention is required unless the above is ineffective or the patient develops a second spontaneous PTX.
I'll join the "I can't see the pneumothorax" club. Regardless, I believe you, and will assume there is one there...
I would favor intervention, at this point, and agree that starting with air-evacuation via thoracentesis is very reasonable. If that fails, then I would put in a chest tube.
I know the cxr doesn't project well. If you look on the lower r you can see a straight line below the diaphragm, which is the lower edge of the pneumo, and the upper yellow bar is indicating the upper edge. It is slightly more than 30%.
Hi, I'm a pneumothorax patient, just discharged from hospital. Had chest tube inserted first, and then VATS done.
My question is, I am passionate about flying, and already secured a place in the undergraduate program in Bachelor of Science (Aviation) in Perth's Edith Cowan University, which includes Commercial Pilot's License. They are waiting for my acceptance. Do I still have the medical conditions and requirements to fly?
Post a Commenttest post a comment