His dyspnea worsened and he was admitted and then intubated. His condition worsened.
For instance, here is a chest xray from one of the ICU days (the sub-cu air is from chest tubes after the VATS.

He did not respoond to steroids and the micro workup was unremarkable. He died after 2 months on the vent.
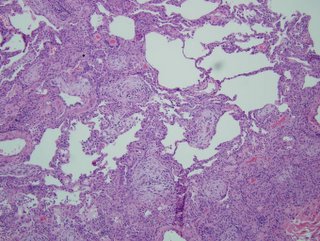
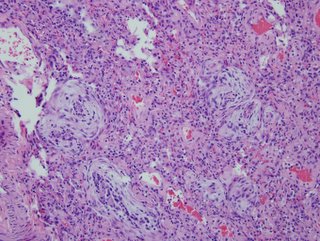
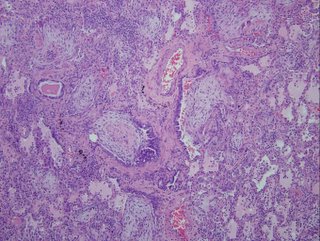
Here are the biopsies:

I realize there may be no pathologists out there reading this, but what would be your top diagnosis (and I'll post answer later in the day).
3 comments - CLICK HERE to read & add your own!:
I am, in fact, about as bad a pathologist as one can find-but I'll take a stab. There's diffuse cellular infiltration of the interstitum, and those look a lot like multiple large granulomas. I'm presuming that special stains are negative, so my best guess here is HP or Sarcoid. Given the failure to respond to treatment, I think that enemic fungi is possible as well--did he receive anti-fungals?
Jeff H and I went to the same path school... The images are very cellular with no intact aerated air spaces. No wonder oxygenation was a problem. In addition to the granulomata, I see hyaline eosinophilic material filling what seem to alveolar spaces and the airways are plugged up with cellular debris. Maybe we are seeing DAD complicating granulomatous infection/inflammation...
Good general comments. As per pathologist interpretation, the diagnosis is essentially BOOP (idiopathic, i.e. COP) with no infectious etiology. This is surprising, considering his lack of responsiveness to high dose steroids (as well as every antiobiotic known to man)...
Here's the reading in unabridged form:
Both lung biopsies of lingula and left lower lobe show similar histologic features of organizing interstitial pneumonia, which is extensive involving the most of lung parenchyme sampled. There are bronchiolocentric granulation tissue plugs obliterating some alveolar spaces and bronchiolar lumen. Rather diffuse interstitial widening with scattered lymphoplasmacytic infiltrates and swollen pneumocytes are seen. Sparse neutrophils are also seen in some of dilated air spaces. Peripherally alveolar spaces are collapsed with fibrosis alternating with distended air spaces presumably due to artificial ventilating aids. Some air spaces are loosely filled with fresh red blood cells. There is no evidence of suppurative inflammation, vasculitis or neoplastic process
Post a Commenttest post a comment