So to make a
complicated story more complicated- when I spoke to our pathologist about the biopsy results he said "I never seen anything quite like this in my career." A prominent lung pathologist from another institution was in agreement.
I've posted their description of the findings below:
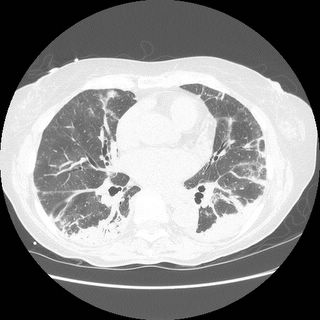
Lung, right, middle lobe, wedge biopsy:
Chronic interstitial pneumonia and patchy interstitial fibrosis; chronic active bronchiolitis with focal proliferative-type bronchiolitis obliterans and organizing pneumonia pattern; focally necrotic granulomatous inflammation.
A constellation of pathologic findings are present in this case. The alveolar parenchyma manifests chronic inflammatory cell infiltrates as well as patchy
fibrosis. Lymphoid aggregates are present, and many of the interstitial cells are plasma cells. Superimposed on this picture are numerous granulomas, some of which show focal necrosis and acute inflammation. A few of the granulomas appear bronchiolocentric. Rare bronchioles contain intraluminal foci of granulation tissue. Special stains are negative acid-fast bacilli and fungi.
The background interstitial inflammation and fibrosis may be related to the patient's rheumatoid arthritis.
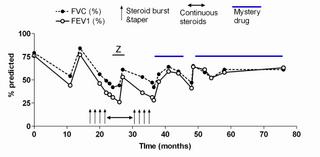
A recent publication
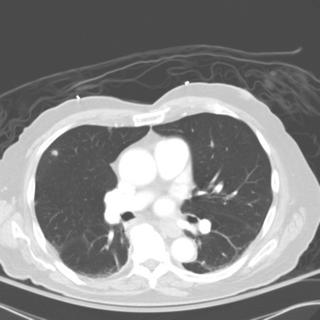
(Modern Pathology 2005 18:651) describes a series of patients who developed persistent pulmonary infiltrates and granulomatous inflammation associated with etanercept use. The histopathologic changes noted in those patients was similar to what my patient had; here is a pic:
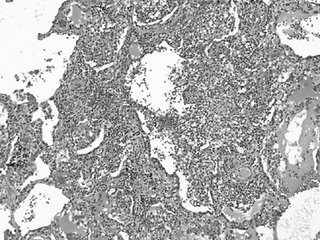
In that series, all of the patients improved with a combination of immunosuppressive therapy and discontinuing etanercept.
This patient has clinically stabilized but has been slow to improve.
Posted by Jennings for Dan.
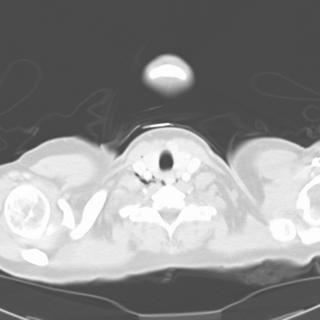




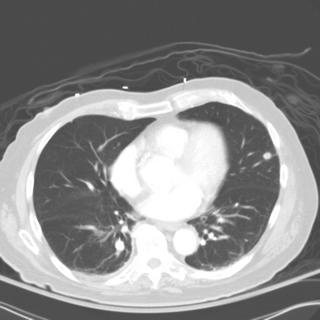
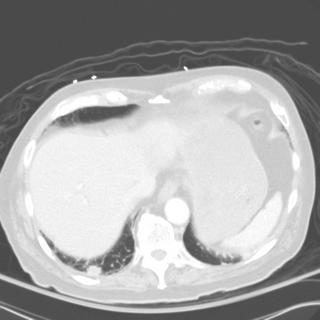
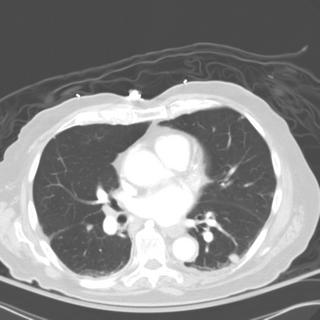
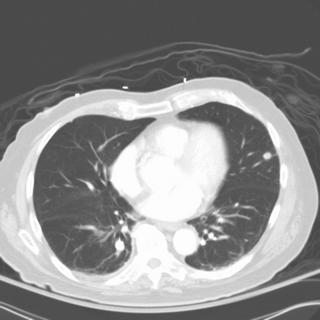
 1 month after stopping the nitrofurantoin:
1 month after stopping the nitrofurantoin: First CXR
First CXR