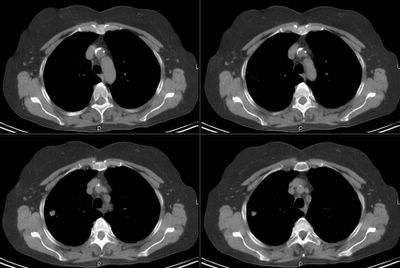
This is a 65 y/o former smoker who was sent to us for evaluation of a pulmonary nodule. She has COPD, has baseline DOE and while having an AECB had a CxR (outside films). The CxR revealed a nodule which is better characterized on the CT below.
She has had no F/C/NS, no hemoptysis.
Her exam was fairly benign. Her FEV1 however, was only 700cc on Combivent?
What would you do next?
Subscribe to:
Post Comments (Atom)
4 comments - CLICK HERE to read & add your own!:
yea, what he said.
I agree with a PET scan and maximal treatment of her COPD to see if there is some reversibility.
If she's not a surgical candidate based on PFT's, quant V/Q, and CPET, than I'd agree with a CT biopsy. Presumably this is a stage IA (looks small, no nodes), so "definitive" XRT would be an option...
We are really on the same page here: I started her on Spiriva, Serevent and gave her 2 weeks of prednisone and got her FEV1 up to 800 cc... There were no nodes on CT and the densities on the CT did not favor a hamartoma.
Her PET scan lit up nicely on the nodule (SUV 7.3) and nowhere else.
A quantitative Q scan revealed 16% perfusion to the R upper lung.
Now what?
A residual FEV1 of ~570 cc is probably too little to resect. Still you could get a CPET to see her VO2(max). I imagine that the surgeons would still find another reason not to operate.
Then, I agree with a CT guided needle biopsy.
Her % of predicted was equally low (<35%)... Her PFTs didnot look good at all for resection. The surgeons, as Lazar suggested were not thrilled with the possibility of resection. I will post the final results later today.
Post a Commenttest post a comment