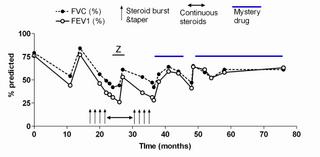
This is not so much a diagnostic dilemma, as a therapeutic curiosity. Think of it as a riddle. This is a very nice lady whom I cared for about 5 years before she was lost to follow up because of an insurance change. She initially came to my clinic after being followed by another colleague who left the University after finishing training. This lady had very severe asthma, with persistent symptoms, and frequent exacerbations that required steroid burst & tapers. She was also quite obese and as a result had some restrictive physiology that was not accompanied by any evidence for interstitial disease on full PFTs and HRCT scans done on multiple occasions throughout the years. After a while I ran completely out of options for her. She was compliant on 6 puffs of Flovent bid, Serevent, Accolate (this was before Singulair), et., and was still ending up in an emergency room every 4-6 weeks.
I started her on a drug that we shall henceforth refer to as "Mystery Drug". I had a biologic rationale for it, but NO DATA whatsoever, other than I knew it to be acceptably safe. I will see if anyone can guess what I started her an and why, then post some follow up.
6 comments - CLICK HERE to read & add your own!:
Doug, we've discussed this case before, so I won't give away the "mystery drug." I do think that this case revisits one that we've discussed before one this blog regarding "refractory" or "difficult to control" asthma. (See the case titled "Reactive Airway Disease? http://pulmonaryroundtable.blogspot.com/2005_06_01_pulmonaryroundtable_archive.html)
So, for the sake of discussion (without going into treatments), how were "non-asthma" mimics and other "causes" of treatment failure evaluated- (i.e. laryngeal dyskinesia, psychogenic dyspnea, non-compliance with standard therapy, CS, ABPA, CHF, mitral stenosis, to name a few)?
Are there any clues in the history you provided to indicate *which* steroid-sparing drug she was on? If not, it could be any none-standard but anti-inflammatory med:Methotrexate (but I don't think the effect is very large, if I remember correctly); Azathioprine would be a good guess since you said you chose something with no data to support it; Chloroquine (very spotty data to support this); macrolide (because of the anti-inflamm component or perhaps because of MAC according to the researcher in Denver - what was his name?); I'll avoid things like an oral leukotriene receptor antagonis since that has data behind it;
You didn't mention anything on IgE levels but I will add Xolair to Jennings' list. I like Jennings' suggestion of a macrolide since there is biological data for other airway conditions but it is not as solid data in asthma.
GERD treatment could improve asthma control as well but then you wouldn't be talking about the biological rationale...
Was she post-menopausal? There are small series on asthma control worsening in post-menopausal women...
And there IS data on Xolair so I added it only as another steroid-sparing agent...
Interesting. On the one hand there is no "data", on the other hand it sure seems to fit Kosh's postulate pretty well.
Post a Commenttest post a comment