Mrs. A is a 34-year-old African-American female with multiple ER visits for pain and also diagnosed with heart failure. She presented with lower extremity edema, increased abdominal girth, and chest x-ray with some interstitial markings. CT scan of the chest (performed for PE). She has dyspnea on exertion which is not prgressive as per patient. SHe requires home O2. She also has a nonproductive cough.
She has noted splenomegaly and pancytopenia for over 10 years when I contacted him.
She takes no medications. Currently she is not compliant with oxygen.
SOCIAL: smokes age 21 to 28 one PPD. She drank approximately 6 drinks per day from age 21 to 25. She has never used inhalational or IV drugs. I have specifically asked if she used crack cocaine, inhaled heroin, or IV drugs. She denied all the above. She is not married.
BP is 97/65 consistent with the prior evaluation P of 90, R 20, body WT is 137 lb or 62 Kg. ENT: There are no oral wounds or lesions. There is no ENT or supraclavicular adenopathy. Lungs are clear bilaterally. Cardiovascular no rub, murmur, fixed heart sounds. Her belly is benign and nontender. There are lower extremity skin wounds, approximately 1 cm skin wounds, but multiple bilateral lower extremities below the knees. She does have a silver-plaqued wound on her lateral right lower extremity. Extremities: There is some lower extremity edema, trace
similar to my prior evaluation in the hospital.
echocardiogram 5/22/2005 - PA pressure 48. Normal EF. Mild tricuspid regurg and she has a dilated right ventricle. Her bubble study was positive.
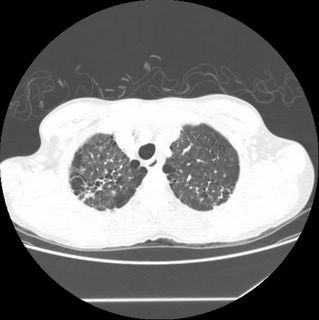
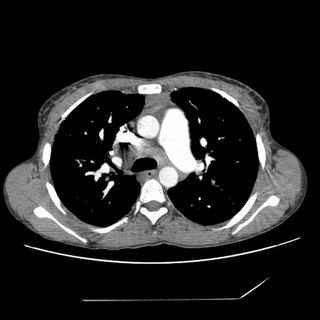
Click to enlarge:

Labs and bronch findings:
WBC 1.9 with 84% Neut. Hct 32 with MCV 74.
SGOT 69 [15-35] SGPT 23 [10-40] TP 8.3 albumin 2.9 BILIRUBIN, TOTAL 1.9 ALKALINE PHOSPHATASE 413
normal creatine and bicarb.
ANA, RF SCREEN Negative
ACE level 205
Bronchoscopy with endobronchial and transbronchial biopsies revealed:
A. Lung, endobronchial biopsy: Active chronic inflammation. See comment.
B. Right lung, middle lobe, transbronchial biopsy: Single poorly formed
granuloma.
Special stains on A B: Grocott stain: Negative for fungus AFB stain: Negative for acid fast bacilli
COMMENT on biopsies:
There is active chronic inflammation in specimen 'A' with squamous metaplasia. A single subtle granuloma is seen in 'B'. The histologic appearance is not characteristic of sarcoid. The histologic findings favor an infectious etiology.
Any thoughts on diagnosis and suggestions for further investigation (especially in light of the interesting TBBX interpretation)?
7 comments - CLICK HERE to read & add your own!:
In a 34 y/o woman with skin changes and some areas of fibrosis on HRCT, along with moderate pulmonary hypertension by echo, one has to think of collagen-vascular diseases, especially scleroderma.
That said, some other features stand out: the upper lobe involvement with what looks like some honeycombing and some ground glass (although based on the one cut I may be overreading this), is an atypical distributaion. What did the lower lobes look like?
Also, the subcarinal LAD would not be typical for collagen-vascular disease.
When you say the bubble study was positive, was it interpreted as an intracardiac R -> L shunt or intrapulmonary? The right sided pressures are not so high that I would expect an Eisenmengers syndrome...
The chronic anemia and neutropenia are also atypical, and suggest a systemic disorder.
The transbronchial biopsies are non-specific. Except to say that the lack of granulomas makes sarcoid less likely, I would not over-interpret.
My next steps would be the following (in no particular order)
-autoimmune serologies
-right heart cath with ventriculogram
-pulmonary function studies
-consider a skin biopsy to evaluate for vasculitis
-surgical lung biopsy
I agree with W/U for connective tissue diseases but I think that Sarcoid is still high on the differential...upper lobe disease, med. LN heart failure which can be due to sarcoid....any W/U done for her splenomegaly and pancytopenia?
Also I agree with the skin biopsy and that i think it should be done first.
I agree with Jennigs's suggestions. Though the granuloma was "not typical of sarcoid", that is a tough call on a single granuloma and in someone with skin manifestations, LAD and unusual lung involvement I would not R/O sarcoid quite yet. As Jennings suggested, VATS lung Bx would be really helpful in making that differentiation.
I did not see a lot of excess soft tissue in the mediastinum, but the PAs in the first soft-tissue cut looked smaller than I would expect. With suspicion for granulomatous infections, I would add fibrosing mediastinitis to the DDx. In-situ chronic VTE/PA microthrombi could lead to that almost "mosaic" aspect on the lung window. It may explain the granuloma without evidence of organisms. P-Agram would be very helpful and I would also get Hysto Ag and serologies.
I am truely hurt that you would confuse me with Jennings....
Yeah, I thought that was kind of funny. I'll be happy to take credit for your comments though.
Oops...
I meant to say I agree with JH's suggestions and how come Jennings hasn't written anything.
This would be a nice case of Felty's syndrome if the patient had a positive RF; although rare, I suppose that you can have Felty's with a normal RF.
In lieu of the pancytopenia and the worry for fungal disease, a bone marrow biopsy may be helpful as well. I presume a hematologist has seen her in the past given this CBC finding. If not, I might consider this procedure before JCH's list.
Post a Commenttest post a comment