We were asked to see this 34-year-old woman for chest pain, dyspnea and persistent fevers. She has a history of adult-onset type I diabetes and presented with significant body aches, pains, fever, loss of appetite and was found to have diabetic ketoacidosis. She was admitted to the intensive care unit, started on aggressive fluid resuscitation and glycemic control with insulin. Her DKA resolved completely. On admission, she had 1/4 blood Cx bottles + for Staph. aureus (MRSA). She had a small L pleural effusion, was given ABTx and a 2-D-ECHO was negative for vegetations.
On the day of this consult, she was much improved but still has some pleuritic chest pain. This was more pronounced on the left but she described it radiating across the chest. No significant cough. No throat soreness. No dysphonia. She also had some diffuse mild abdominal pain and diffuse mild abdominal tenderness. No nausea or vomiting. She complained of let leg pain and could not weight bear.
On exam, she appeared ill, was febrile. HEENT was unremarkable. She had a L pleural rub. Cardiac exam was unremarkable. Abd was diffusely tender with no focal findings, no guarding or rebound. Her left thigh had normal skin but the lateral aspect felt almost indurated to touch compared to the right. No erythema, no rashs, no warmth and only tender to deep palpation.
I reviewed her data and she had had intermitently + blood Cxs for Staph aureus (2/6 bottles) and a urine Cx also + for MRSA despite a few days of IV vanco.
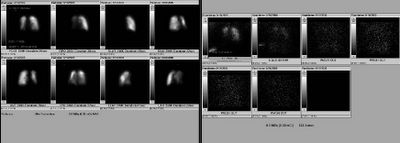
Her CXr is seen below. They had already done a V/Q which I have attached. All those deffects are matched. What would you do next? What is your DDx?

Follow-up/answer to case on http://pulmonaryroundtable.blogspot.com/2005/07/follow-up-to-staph-infection.html
4 comments - CLICK HERE to read & add your own!:
Was the left leg a cellulitis or was it overlying skin changes in the setting of leg swelling. In other words, did you rule out a DVT? I realize the v/q was matched (was this read as low prob?), but p.e. might still be considered. In terms of the plurisy and b/l parenchymal abnormalities, an autoimmune disorder, notably lupus, might be considered. The staph would then merely be indicative of her underlying diabetes. So I would get an ANA to see if that's a path worth taking. Again, some of this (like the abdominal discomfort and the staph and cellulitis) might just be the diabetes, instead of trying to tie all of that together. I'll wait and see what others think...
The leg actually had no skin changes so DVT is a good thought but there were no changes of cellulitis.
I will wait for a few more comments and add some more info.
The resolution on the CXR is absolutely terrible on my machine. Is there a loculated lateral pleural effusion, or is this just scapula?
Given all of this MRSA documented, I would first get a plain film of her LLE. Maybe you will get lucky for an appearance of osteo or soft tissue infection.
If that is negative, I would consider a CT scan of the C/A/P/Lower extremities (maybe consider PE protocol if radiology feels that you can get all of the necessary information) looking for an abscess or other endovascular source of infection.
The resolution of the CxR is truly bad, Mike. She does have a loculated effusion. e Tap'ed that and it was exudative but not an empyema. Dopplers of lower ext. were negative for DVT. Her CP and dyspnea improved with the thoracentesis.
I will post the w/up on the leg and the MRSA tomorrow.
Post a Commenttest post a comment