He presented with fevers, SOB and cough productive of thick purulent sputum and had a LUL infiltrate with sputum Cxs positive for MDR Pseudomonas aeruginosa. Imipenem and APAG had the best MICs though it was also SS to Pip/Tazo (resistant to everything else.
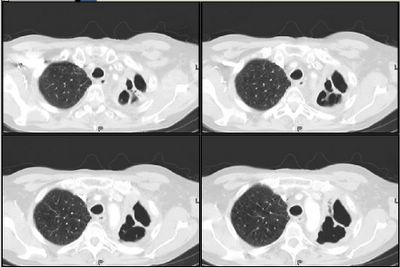
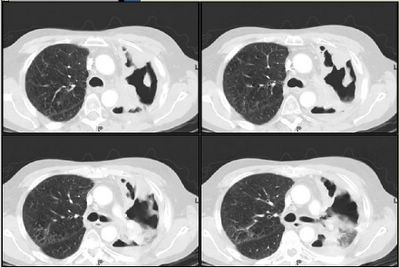
He has received 2 weeks thus far of Imipenem, Amikacin and aerosolized colistin. He is stable but still has copious purulent sputum production and his sputum samples remain positive for Pseudomonas. His CT scan now shows extensive damage to the LUL (previously devitalized by xRt) :
 Susceptibility profile has remained the same. Would you add or change anything at this point?
Susceptibility profile has remained the same. Would you add or change anything at this point?
5 comments - CLICK HERE to read & add your own!:
I think that the key is clinical stability. Is he still febrile? I'd hold the line and continue with the current drugs. It looks like it's probably necrotizing, and will take a long time to resolve.
I agree with Jeff H and would continue antibiotics for roughly six weeks and reassess with a CT scan.
Looking at that CT and realizing that he has had radiation, he may ultimately need a bronch to define the anatomy of his LUL. I would be very worried about an endobronchial lesion or XRT stricture. If he has a significant stricture and this pneumonia (i.e. his secretions) does not resolve, I would ask T-surg to see if they can get a rigid bronch and a stent into that area. Alternatively, a palliative lobectomy may prevent him from drowing in secretions that cannot drain appropriately Developing a unresolving post-obstructive pneumonia with continuous infectious symptoms is a miserable way to dye.
2 Questions: Does he have disease outside his chest and what is his performance status?
Very good points on the necrotizing aspect. Unfortunately we have two other patients now with similar Pseudomonas isolates: another lung Ca with a destroyed RUL and a patient with quadriplegia and therefore poor pulm clearance. All 3 have been on combination Tx.
Sadly, the patient in this case had sudden massive hemoptysis this am and died within minutes before even a code could be called. He probably ruptured a large vessel in the necrotic space... His most recent sputum samples (after 18 days of Tx) were still positive for Pseudomonas.
That's too bad...will an autopsy be done? And it sounds like your hospital may need some infection control people to do some investigation...
The interesting thing is that each of these Pseudomonas isolates has a slightly different susceptibility pattern (gent vs amikacin, etc.) from each other but they are all quinolone and ceftazidme resistant.
Post a Commenttest post a comment