His PCP initially ordered an abd u/s which was normal. He was placed on 2 different antidepressants with no relief. A referral to a gastroenterologist is pending.
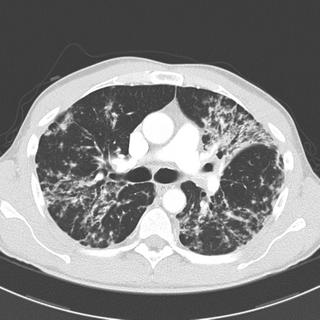
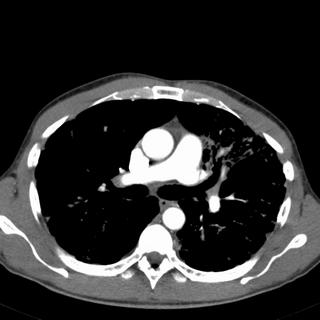
A CT of the abdomen was performed. It was normal except some abnormalities seen at the bases of the lung. This prompted a CT chest. Representative cuts are below. He was referred to me for this.
PMH: None
PSH: None
SH: Never smoker, drinks rarely. Police sergeant in a major city. No drugs (confirmed by 7 years worth of random drug tests that his PCP sent to me from his police precinct). He denies any drugs other than marijuana prior to 7 years ago).
PE: Crackles in the mid lung zones
Spirometry: FEV1 92% predicted
FVC 85% predicted
FEV1/FVC 108%
Radiographs:



What next?
11 comments - CLICK HERE to read & add your own!:
The pretracheal lymph node on the mediastinal window seems borderline enlarged (Probably less than 1 cm).
While the differential here is long, I tend to believe that this most likely represents Sarcoidosis. Whatever it is, I would start with doing bronchoscopy with Bal/TBBX/and EBBX. I may attempt WANG as well if we can see more lymph nodes on additional cuts. I would send the BAL fluid for cell count/diff (also CD4/CD8) and especially cultures, , as TB is also a possibility here (high risk job for TB).
Well, we have a mid/upper lung- predominate process with relative sparing of the lower lobes. I agree that sarcoid is a possibility. I really don't see any adenopathy though. I would expect that someone with stage IV sarcoid would have symptoms. Other upper-lobe ILD's such as eosinophilic granulomatosis are less likely with his non smoking status but HP cannot be ruled out - is there anything on history to suggest exposure to antigens associated with HP? Also agree with Krayem about TB since TB is not exactly rare in the area in which this patient worked.
But before a big work up with brinch +/- open lung biopsy; does he have old films? It would be nice to know if the change radiographically coincides with his weight loss over the past 4 months or if he has had these findings for years.
I agree that this is most likely sarcoid, with EG, HP, and TB also possibilities. I do think that the pre-carinal/pre-tracheal node is enlarged, increasing my suspicion for sarcoid.
Just to add to this a bit, I'll through out the possibility of multi-focal BAC carcinoma as well. I agree with old films, bronch, biopsies, and culture.
Aside from his weight loss, he doesn't "pulmonary complaints" such as cough or sputum production. Although the lack of complaints would not translate to the lack of infectiousness if he does have TB, I think that our overall low clinical suspicion combined with the apparant chronicity of the CT scan changes (i.e. lack of focal/cavitary lesion), would allow us to hold off on 4 drug treatment while persuing a definitive diagnosis.
However, I would absolutely not treat for LTBI if his PPD is positive. If his PPD is positive, then I would consider 4 drugs pending cultures from induced sputum or BAL.
PPD is negative. Checked in PCP's office and has been negative yearly via the police health records.
I tried every question I knew to get any exposure history. Nothing. He is a couch potato, lives in the big city (clean house, no "pests" or pets), works a lot of hours (his main job is desk related, but frequently "walks the beat."
I bronched him with BAL and 9 TBBx (good sized pieces). Caused a PTX too. BAL showed rare MSSA. TBBx results:
MICROSCOPIC DIAGNOSIS:
RIGHT LUNG, TRANSBRONCHIAL BIOPSY
--- LUNG PARENCHYMA WITH SINGLE NON-NECROTIZING GRANULOMA
--- NO MALIGNANCY IDENTIFIED Comment: Level 2 shows a single small non-necrotizing granuloma. Special stain for acid fast bacillus is negative. Grocott stain for fungal organisms is non-contributory as diagnostic tissue is not present on the slide. Negative staining results do not rule out respective infectious etiologies. Sarcoidosis is also included in the differential diagnosis. There is no other pathology identified in this biopsy material.
Would you treat the MSSA?
Would you treat this as sarcoid?
I would not treat the MSSA and call that a contaminant. I would consider this sarcoidosis and treat him as such (high index of suspicion, compatible CT and biopsy). the CD4/CD8 ratio on the BAL could be of some help. I would have obtained endobronchial biopsies (carinas) to increase the yield. I would also now get calcium level (serum and 24 hour urine) and ACE level, and eye exam.
I would not treat the MSSA.
This looks like sarcoid and he has essentially normal spirometry (althought the FVC is low--do you have a full set of PFT's). He's asymptomatic. I would probably not treat at this point, and follow clinically and with full PFT's followed by spiro with a DLCO over time. If this is progressing, then I'd favor a repeat bronch and, if negative, consider a lung biopsy.
I would not treat (for his sarcoid) unless PFT's change or he becomes symtpomatic. I would also add (regarding calcium, eye exam etc) to get an EKG. Cardiac sarcoid is rare but the most common presentation for cardiac sarcoid is sudden death (from an arrythmia).
I think that there are enough symptoms to treat as sarcoidosis. The most obvious is weight loss (constituve symptoms from sarcoid are not unheard of), besides the "bronchiectatic" changes. as far as waiting for cultures, I guess the concern of the author is about using steroids in somebody who may be infected. Well, I would treat now, but probly with plaquenil (which may work for constitutive symptoms), especially if he turns out also to have hypercalcemia or hypercalciuria, whithout having to worrry about the culture results 6 weeks down the road.
The weight loss and a presumptive diagnosis of sarcoidosis may be true-true and unrelated. I'm not sure we can attribute the weight loss to sarcoidosis, and would persue a definitive diagnosis prior to treating. The one "non-caseating granuloma" in this patient would not be sufficient for me to treat.
No full set of PFT's yet; awaiting the PTX to completely heal prior to having him go through this test.
As far as the MSSA, DA, would you still treat if he had no PMN's on the gram smear and the gram stain showed no organisms? I agree with the staph + bronchiectasis = badness so I do not want to drop the ball on this one.
Fungal cultures negative; AFB smear negative and cultures NGTD after 3 weeks. Calcium is normal. EKG is normal.
He is getting an EGD & GI w/u next week to confirm that the weight loss is not GI related.
I still think treating stage III sarcoid with a short course of prednisone (at doses no higher than 20 mg/day) may be the right thing to do. His xrays are really ugly and I would hate to repeat PFT's in 6 months to show a FVC of 75%.
That being said, waiting 3 months would be ok with me too.
Post a Commenttest post a comment