
As a reminder, this is her admission cxr. Her chest CT's shown in the original post are 2 months apart.
An echocardiogram showed EF 50%, moderate mitral regurg. No vegetations.
In sum (after original admission described above), this woman has been in and out of the hospital with episodic SOB and CXR's showing the fluffy infiltrates. Each time, her BNP was elevated and the troponin was high. On the other hand, she would have hempoptysis. The primary team treated with both lasix and steroids, making it diffucult to distinguish between cardiac origin and a vasculitic picture. She had an open lung bx:
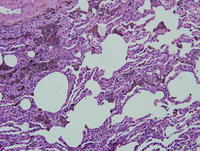 .....
.....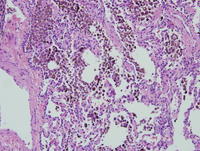
This was read as lots of hemosideran-laden macrophages but no evidence of capillaritis or vasculitis. A swan was placed based on the echo. It showed big V waves consistent with severe mitral valve regurgitation. The previous echos underestimated the degree of severity, apparently. She had her mitral valve replaced and all of her symptoms essentially resolved. The steroids and lasix were stopped and she continues to remain asymptomatic. Her latest CXR is shown here.
So in sum this:

is from mitral regurgitation. Bloody aveloar filling can be from capillaritis as suggested by her high anti-cardiolipan titer, but the biopsy showed hemosid-laden macs which just means that macs were eating blood not that there was any vasculitis. Replacement of the valve solved the problem.
My little lesson for the day: the whole autoimmune angle was a red herring. It was not active. The only positive results we have are a high titier and a sed rate of 100. The U/A was negative. The other titers were negative, etc. Before the valve was replaced, she was likely respondign to the diuresis, not the steroids.
8 comments - CLICK HERE to read & add your own!:
It turns out your wild a** guess #1 was the top of the list for the primary pulmonologists as well. The other thing was that she had mitral regurg on an echo. So we have 2 things that can cause hemoptysis - one responds to steroids and the other responds to diuretics. She got both at the same time. It led to a lung biopsy after tbbx were nondiagnostic. The histo should be arriving shortly; after I post it I'll wrap up the case along with one additional test that ultimately gave the answer...
Great case.
In terms of Doug's 3 things on the differential diagnosis, I have a question:
Would idiopathy pulmonary hemosiderosis or pulmonary veno-occlusive disease respond that rapidly and completely to steroids?
(i.e. sats of 95% on RA after steroids)?
The rash would be unexplained by these diagnoses as well.
My vote is for MCTD with associated lung involvement.
Any results on the other antibodies we've asked?
The scl-70 was negative. The rest were not sent for.
For Lazar: idiopathic pulmonary hemosiderosis is a rarity, and it is not known to be responsive to steroids although (imagine this) steroids remain the standard of care. It's usually diagnosed in kids/young adults.
Similarly, pulmonary VOD should not really be steroid responsive.
I agree that the rash is unexplained by mitral valve disease, as is the elevated ESR. I suppose that it's hard to argue with the outcome, but I wouldn't be terribly surprised if the patient has a similar presentation somewhere down the line.
I agree with Jeff H: sure she had pulm edema and got better with the MVR but that doesn't explain the rash and the ESR of 100. She probably has an underlying vasculitis associated with the ACL independent of her mitral disease.
The biopsy does not support the idea that the abnormal cxr was due to a vasculitic process. There is no evidence for capillaritis. There is no arguing that she has an autoimmune disease - she has a esr of 100 and an anti-CL antibody. However, there is no evidence that her pulmonary presentation was due to this.
Post a Commenttest post a comment