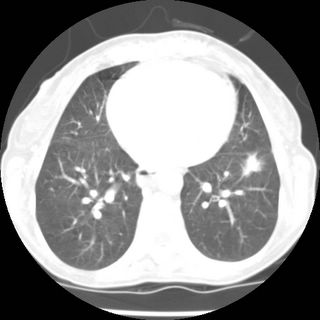
What would you do with the following patient: she's a 60 year old lifelong nonsmoker with quite minimal respiratory symptoms who was referred for nodule picked up accidentally during a hospitalization for small bowel obstruction (due to adhesions from a prior surgery). The interesting thing is that her PFT's showed significant obstruction (FEV1/FVC 59.1 (76%) FVC 1.47 (56)%, FEV1 0.87 (43%) TLC 75% ERV 114% RV 98% RV/TLC 135% predicted. DLCO 76% DL/VA 130%;
her height is 147 cm and weight 41.4 kg) and even her CXR

looks like emphysema. Remember also that her symptoms are minimal. So what do you make of this?
The other problem was the original reason for referral. A lung lesion in the lower lobe. Looks pretty nasty and spiculated
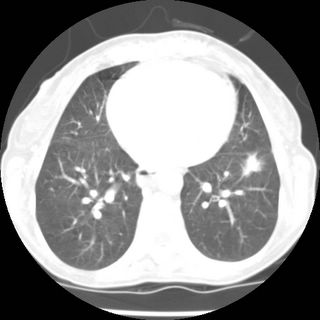
but the PET was negative and there has been no change in size compared to a CT done 6 mos earlier. What would you make of the PET-negative lesion and what would you do about it? (i.e. take it out in a nonsmoker in case it's BAC) or follow it.
7 comments - CLICK HERE to read & add your own!:
In conjunction to Doug's reference, I refer you to a website:
www.chestx-ray.com
On this site, you can calculate the pretest prob of malignancy (the bottom calculation) and plug the patients' characteristics and nodule information in the top to get a post-test probability of malignancy.
When done for this patient, the post-test prob of malignancy is 0%. This is a nice program to allow you to get some objective info on a patient and a nodule.
Now the case... she has a restrictive vent defect too as her TLC is 75% predicted. Can we have some more history?
Given the degree of obstruction she has on spiro, I would expect that she has more air trapping or a reduction in her DLCO. Maybe this is asthma and would get better with steroids.
www.chestx-ray.com is really a great resource and the stats help put things in perspective for some patients. Any chance she has had unrecognized asthma and now has airway remodelling?
Any Hx of second-hand TOB or interesting occupational exposures?
I actually put in a "non-malignant" growth rate as the nodule had not changed in 6 months.
If I put in a "not known" the risk of malignancy is 3%
Here is my criteria:
Pretest prob 18%
Nonsmoker, no hemoptysis, no prev malignancy
1.1-2cm, lower lobe, spiculated, growth rate not known, no cavitation, no calcification
contrast enhance not performed, neg PET.
Did I enter something incorrectly?
Well, I see carlos has posted his case so hopefully you all won't give up on my case just yet. Here in answer to your comments. We will start with the PFT's.
1. regarding asthma; she has had 2 post-bronch studies that showed no significant respponse (FEV1 from 0.87 (43%) to .99 (49%)). We did put her on inhaled steroids anyway, but repeat spiro showed no change in the severe obstruction. It's a good point about post-op and surgery, but repeat sprio a year later showed the same defect. Also, her FEV1/SVC ratio was no differetn than the FEV1/FVC ratio.
2. regarding emphysema; the rest of the CT does not show any emphysema or bullae. The alpha 1 globulin level was normal, making A1AT deficiency unlikely. Her occupational and social history are unremarkable.
2. As for the suggestion that she also has a restrictive defect; there's not much on history to suggest an etiology; she has no weakness, she has no heart failure, her CT shows no parenchymal disease. She did have some pleural effusions in the setting of the abdominal surgery but a CT later showed complete resolution without evidence of pleural abnormalities. Actually, come to think of it, I never repeated that TLC - maybe there was some residual effusion during that sprio - I will have to check. good point lazar.
Her abdominal story is she presented with n/v with gastroenteritis. Found to have a partial bowel opbstruction and got laparotomy with lysis of adhesions. No one knows waht caused the obstruction as far as I can tell from the notes.
As for PET discussion: doug asked about change in size in order to help figure out the pre and post test probabilities; the latest CT shows it to be 1.7 x 1.0 cm with no change at all compared to the one 6 months ago. BTW a CXR from 7/2004 was negative.
A CT (her first) from 12/04 is not available to check for change in size; the report says it is "about 1.5 cm" but I am not sure if this is a true change.
Jennings measurement of 17 mm gives a pretest prob of 22%.
That gives a post test prob of 4% malignancy.
What is a nice learning point for me in this case is how the size of a nodule really affects the decision pathway.
Even in lung cancer, size does matter.
As for the patient, any chance she may have HP? A subset of patients with HP will have both obstructive and restrictive physiology. In Farmers lung, for ex, obstruction is more common than restriction
Cormier et al. ERJ 2000. 16(1) 56-60
Well, there's nothing on history to suggest HP and the CT does not show anything like ground glass. I admit thought that I didn't get an HP panel. In patients with obstructive HP, do those patients have classic ground glass findings like the restrictive cases?
Actually, no.
They can simply have findings on the CT that look like classic emphysema. Their disease likely starts as bronchiolitis, so I suppose that you can see a mosaic pattern on the expiratory images if you obtained a HRCT.
Another diagnosis to consider if you are still not sure is idiopathic bronchiolitis obliterans. A SLB would be necessary to diagnose this.
Post a Commenttest post a comment