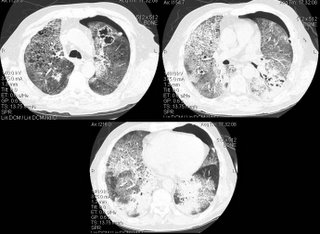
A few weeks later, he was admitted to another hospital with continued dyspnea, and transferred to our institution, where he quickly developed respiratory distress. The following CT scan was obtained, and he was transferred to the ICU.
Questions:
1) What intervention led to a rapid improvement in this patients acute respiratory decompensation.
2) What is the the differential diagnosis for the other two findings on this CT scan
3) What steps would you take to further evaluate and treat the patient?
7 comments - CLICK HERE to read & add your own!:
Well, first treating the Pneumothorax will improve his symptoms.....
second: he has boopp injury pattern on biopsy that is steroid nonresponsive..I want to R/O infection first
What is his immunological status?
Yes, he felt much better after chest tube placement.
As far as we know, he is immunologically normal. He has no history of skin or sinopulmonary infections. He has children.
For the sake of arguement, let's presume that we don't know the previous biopsy "results."
He has been bronched before, and no infectious organism has been found.
He has had two previous CT scans over the past few months, and each was consistent with the shown CT scan; one exception is that the cavitary lesion is new.
It is more informative for me. This is indeed a help to people who are not aware of their conditions. At times potential diseases comes subtly causing us to relax. When the disease is already critical, that is the only time we worry. The good thing is that concerned people are willing to provide the necessary information.
DDx includes lymphangitic spread, DIP, NSIP, LIP, UIP, sarcoid, WG, etc. Would get serology and UA (RBC casts). Anything suggestive of malignancy on routine labs or mediastinal/hilar LAN on mediastinal windows ?
To add: It almost looks like crazy paving (ala Pulmonary alveolar proteinosis), but the cavitary lesion would not support this.
How about CMV? Was the shell Ag found in BAL?
Sorry I didn't update this yesterday--I'm in the process of moving and away from my computer.
Nice comments. All serologies, including ANCA and anti-GBM have been negative. There is no history or findings on the biopsy to suggest malignancy.
So, to bring it all together, our first goal (after placing a chest tube) was to obtain the slides from the surgical biopsies. These were reviewed with our pulmonary pathologist, who felt this was, indeed, PAP (pulmonary alveolar proteinosis).
There is a third diagnosis as well. BAL fluid grew out Nocardia.
So, three diagnoses:
1. Acute Pneumothorax
2. PAP
3. Nocardia (presumably due to the steroid-induced immunosupression).
The patient is now on Bactrim, and plans are underway for a whole lung lavage.
Post a Commenttest post a comment