This is a 60 y/o man with a 50 p/y Hx of smoking sent to us because of worsening DOE, cough productive of scant amounts of thick sputum and weight loss. No hemoptysis, no CP.
PMHx: Mild HTN.
SHx: 50 p/y TOB. Quit in 2003.
On exam, thin male in NAD. Distant BS B/L with rare R upper crackles. S1/S2 RRR, benign abdomen.
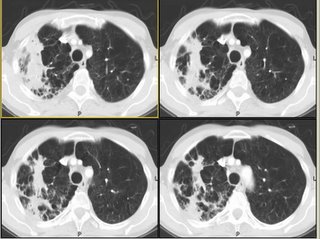
His Spiro revealed an FEV1 of 1.1 L (27% of his predicted) and he had the following CxR and CT scan findings:

update(after 1st 2 comments):
He was started on aggressive bronchodilator therapy, given ABTx and steroids and returned with symptomatic improvement. His FEV1 increased to 2.17L (53%) and he felt better. However, he still had some weight loss (6 lbs.) and a persistent infiltrate after 4 weeks. I did a bronch which revealed only chronic bronchitis and no other Dx.
A PET-CT was done
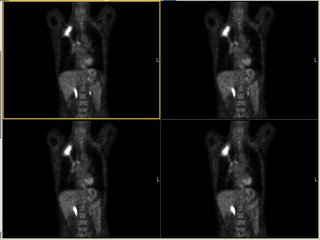 and it revealed marked FDG uptake to the RUL (average SVU of 13 with max SVU of 21) and nowhere else. What would you do next?
and it revealed marked FDG uptake to the RUL (average SVU of 13 with max SVU of 21) and nowhere else. What would you do next?
3 comments - CLICK HERE to read & add your own!:
Greetings from Brazil.
I actually left this case ready so I wouldn´t have to type much. I had the same concerns as Doug that this looks like CAP but Lung Ca is always a concern. I didn´t put all the CT cuts but some of the more posterior and lower process (rather than all the scarred up lung) looked a bit like soft tissue density.
Well, despite the positive PET, I would agree with Doug that TB is still quite high on the list. However, I assume you BAL'd the RUL without any AFB? A PPD is tempting, but wuldn't help to evaluate for active TB, and latent TB with a scar shouldn't be PET positive.
I realize that carcinoma can never realy be ruled out, but the shape looks funky - not mass-like (the air space part could be seconary infection so this can't be used to r/o underlying cancer).
I might get a split-lung perfusion or something similar and if operable, might bite the bullet and resect.
(disclaimer: the way the email was set up, I did not look at the answer; parts 1 and 2 are separated by enough space in the email that it was easy not to cheat) :)
From Carlos: with a positive PET, improved PFTs in a smoker with ongoing weight loss we went ahead with surgical resection. He did very well post-op and the lesion was an inflammatory mass with no clear etiology but some Actyno-like filaments on path (though not on Cxs). He remains on bronchodilators, has gained 13 lbs from his weight nadir and other than thoracotomy site discomfort has no other complaints.
Post a Commenttest post a comment