We thought, given the mild eosinophila, his immigration history, and the cystic appearence on CT scan with what appeared to be multiple septae, that this could very well be an echinococcal cyst. Other possibilities included malignancy (esp sarcoma), or sequestration (although we did not identify a feeding vessel). I did not show it, but there was one 2 cm calcified lesion in the liver. So, I presented his case to thoracic surgery for primary resection. Our surgeons asked for an ID opinion, which was obtained. Although review of the literature showed that percutaneous drainage may be an option for hydatid cysts in the liver, this has not been shown in the lung. The ID consultants agreed with primary resection, but we chose to treat for 3 months with albendazole first.
Two weeks later, the story changed again. I was contacted by another radiologist (who had seen the initial CT scan in a conference). She sent me some computer reconstructions:

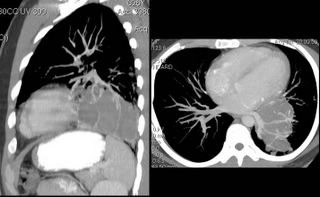
As seen, what we thought were septations were, in fact, vascular branches off of the left pulmonary artery. Additionally, she felt that the fluid density was not cystic (60 hounsfeld units). Now, the possibility of sarcoma came into play.
CONCLUSION: I showed these films to our thoracic surgeon, who again balked, so I rephrased the question. I asked him to name any potential diagnosis of this lesion for which resection was not appropriate management. The patient was taken to the OR 2 weeks later, and a left lower lobectomy was done.
GROSS PATH: multiple cystic lesions containing "thick green and brown material."
MICROSCOPIC DIAGNOSIS: bronchiectasis with eosinophilic abscesses.
There were no parasites seen. There was no fungus. Cultures were negative.
I saw the patient in follow-up last week, and we are both dissapointed at the lack of a definitive etiology for all of this. He feels well, although he stopped taking his meds and his airways obstruction has significantly worsened. He is off of the albendazole, and we have chosen to follow-up clinically and with periodic imaging to identify any potential new lesions at an early timepoint.
Any other comments, thoughts, or suggestions?
5 comments - CLICK HERE to read & add your own!:
Very interesting (if anti-climatic). Do you think he had a resp. tract infection with focal airway damage and intermitent obstruction (like a ball-valve effect) with secretions and progressive destruction and focal dilation?
If that is the case he should do well as the process was very focal.
Any unusual micro isolates?
This was very interesting though anti-climatic. With such a focal lesion it looks like a lower resp. tract infection with focal airway damage and a ball-valve effect with progressive dilation and destruction: the ultimate bronchiectasis.
With focal (now resected) disease she should do very well.
I'd still check him for causes of bronchiectasis (e.g. check immunoglobulins) though it is less likely that he had a systemic process causing only localized disease.
Any unusual micro isolates?
Serum immunoglobulins were normal--I actually checked those after his initial visit before the CT scan. Best I can put this together now is that he had some parasitic infection in the past (still possible echinococcus) that had resolved on its own prior to his presentation, or alternatively we supressed/killed more than we anticipated with the Albendazole prior to resection. No micro isolates have come up yet.
A literature search for eosinophilic lung abscess (excluding all papers regarding CEP, AEP, etc) comes up with one hit in a regional journal from India in 1967. If only I could get that paper....
If the cyst were due to Echinoccocus it would still be fairly easy to diagnose on path even after albendazole. The remnants of the scoleces would be easily identifiable. So even though I'd love to sound smart and have gotten the hidatid cyst Dx, it seems less likely... If memory serves, there are several serological tests for Echinococcus, including ELISA and PCR for peripheral blood but I think ELISA turns negative with treated or "old" cysts.
Actually, the serologic tests have outstanding specificity with horrible sensitivity. We checked them after the CT scan, and they were negative, but it didn't change our approach.
Post a Commenttest post a comment