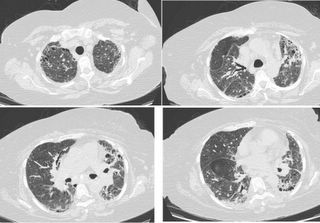
HRCT 2004
An echo at that time showed normal EF with normal-sized RV and RA. BNP 35. Since that time she has had a number of ER visits and 1 or 2 admissions for shortness of breath. Because she never follows up in any clinics, work-up is always ER-limited and treatment is usually based on the old CHF or COPD diagnosis with “pulmonary fibrosis” put into the past medical history, based on above CT. I assume that between visits for SOB exacerbation she is relatively ok, although on the review of systems from one ER note, she “aches all over:” with arthralgias. On SH 1 ½ PPD tobacco. No drugs or alcohol.
On this admission she presented with an hour or so of 9/10 chest pain with dyspnea. Vital signs in ER were 67/46, heart rate of 118, breathing at 22, temperature 36.5.
ABG 7.35/44/43 unknown FiO2. WBC 11. Hct 29. Platelets 200. D-Dimer 1000.
INR 1.15. Cardiac workup was negative.
CXR in the ER:

ER CXR, no change from baseline of 4 months ago
She was put on heparin to cover for PE (later ruled out by CT). She was admitted to the ICU and a day later was intubated for hypoxia. The intubation was difficult. About ½ a day or so later there was frank blood in the ETT. ENT fiberoptic exam showed a laryngeal laceration consistent with intubation trauma. Heparin was stopped and the bleeding stopped. However, over the next few days her FiO2 requirements increased and she required PEEP 15. Here are her xrays during that time:
 Day 1
Day 1 Day 2
Day 2 Day 3
Day 3 Day 4
Day 4Question: What is the cause of the xray findings? What would you do next if you were on rounds? Or you can ask me about any other data you might need.
9 comments - CLICK HERE to read & add your own!:
I think that the differential includes massive aspiration due to difficult intubation or due to aspiration of bloodl This may have resulted in ARDS explaining her severe hypoxia. However, due to her history she may have had DAH especially that she was placed on heparin.
My next step will be BAL. my question is : if BAL is bloody, will u consider it secondary to DAH due to an underlying autoimmune disease or due to massive aspiration of blood?
Agreed. Looks like underlying pulmonary fibrosis--could be IPF, although with the "aches all over" one can easily envision a collagen-vascular etiology.
In either case, this could be pulmonary fibrosis with ARDS-either with a defined etiology or idiopathic, in which case it's AIP or an "acute exacerbation of IPF" aka Haymann-Rich.
If there is evidence suggesting a collagen-vascular disease, this could easily be DAH.
Finally, acute eosinophilic pneumonia could look like this, as could acute (on chronic) hypersensitivity pneumonitis. Neither of these is likely.
I agree with bronch, altough it can be tricky in someone on 15 of PEEP to maintain oxygenation. Also, even in cases of DAH, bronch may fail to show blood in up to 50% of cases. This will let you look for laryngeal blood from the laceration. I'd also try for a BAL for culture, cell count, and differential.
In addition to broad spectrum antibiotics, I'd obtain serologies for a possible collagen-vascular disorder and check urine for red cell casts. If any of these are positive, or if I saw DAH, or if the patient is not responding to antibiotics, I'd probably bite the bullet and give some pulse dose steroids.
1. The blood pressure normalized after a liter or 2.
2 The bronch: clear BAL in to middle lobe, bloodly liquid out. Repeated lavages did not clear the blood. Cell count showed 88% neutrophils. Micro was negative.
3. Labs: ESR 115. ANA, RF and ds DNA negative. Hemosid-laden and anticardiolip AB pending.
4. IPF seems a bit less likely given the distribution - there is more upper than basilar. I guess it's not ruled out but doesn't quite go with current xray patterns.
So, this is DAH. The CT cuts look like interlobular septal thickening with honeycomb change. I guess there could be some ground glass as well. My money's still on a collagen-vascular associated UIP or NSIP, now with DAH. Unlikely to be Wegener's or goodpastures. Still not much history to support RA or Scleroderma.
Looking back at the films, there appears to be persistent elevation of the right hemidiaphram since admission. Is this seen on old films (if available). If so, I suppose there could be a mass in the right hilum-I don't see any evidence of lobar collapse or mediastinal shift to account for volume loss on the right.
I'd try to repeat a CT scan, and barring anything drastic I'd give 1g of Solumedrol a day for 3 days. It may be worth trying for a surgical lung biopsy here, although we all recognize the associated risk of that.
Horowitz suggestion regarding soumedrol x 5 days for DAH was tried. I'll post that succession of post-solumedrol xrays tomorrow.
Any results on ANA, ANCA or anti-GBM?
ANA negative. ANCA and gbm still pending.
Let me add to the differential:
RB-ILD (she is a pretty heavy smoker) with superimposed AIP from a viral etiology. This might better explain the constitutional symptoms leading up to the acute event with the atypical CT for UIP.
Kudos to you for bronching someone on 100% and 15 of PEEP.
"Kudos to you for bronching someone on 100% and 15 of PEEP"
Prior to bronch I was sure it was DAH, but I had to confirm with the BAL. Anyway, her fiO2 was about 70% at the time of the bronch and we did the bronch quick jkust to get the bloody fluid then out.
Post a Commenttest post a comment