reflux, cold intolerance, e.g. coldness/pain in fingers in response to cold, and thickened skin in her fingers. She also reports some dysphagis and a barium swallow in Jamaica, which was consistent with dysphagia.
PmHx HTN and a thyroid problem.
Exam - clear lungs. O/W unremarkable exam.
PFTs - moderate restriction and DLCO 70%.
ANA weakly positive; RF 30 (<15). SSA/Ro antibody negative; Scl-70 antibody negative.
HRCT from Jamaica shows bibasilar some interlobular thickening, some gnd glass and a bit of honeycoming. Rest of the paranchyma was normal or with very minimal ILD findings.
BAL: micro negative. 90 WBC with 95% macrophages.
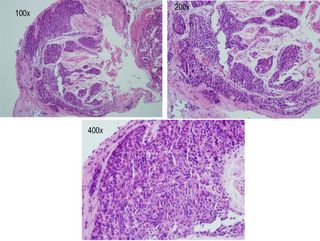
Here is the transbronchial biopsy:
What do you think?
10 comments - CLICK HERE to read & add your own!:
Sounds like CREST syndrome and a centromere test would be appropriate. I don't know what to make of the biopsy.
BTW, I plugged your site on my latest post. I hope it throws some readers your way.
Good case. The biopsies are quite comprehensive for TBBx. I am having some difficulty with the resolution: it seems that all that cellularity is within air-spaces but because of the resolution on the computer screen I can’t really follow the small airways. It seems that there is a an organizing pneumonia and on the right side of the low-res (100x) view there seems to be further inflammation/proliferation in the air-spaces around a couple arterioles.
This could be CREST as suggested with BOOP/COP. Usually we don’t get COP called on TBBx but this seems to be a good size Bx.
Anything on micro stains or Cxs?
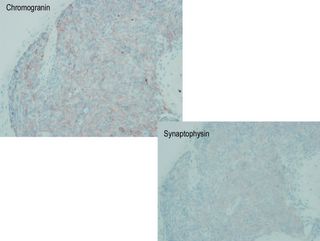
As far as the special stains go: I also had trouble with the Chromogranin staining resolution. It seems that most of these small cells are positive on staining. Is that correct? Chromogranin is located in neuroendocrine cells and would be seen in small-cell. The architecture here seems very organized with individual “islets” of Chromogranin-positive small cells almost looking like a carcinoid but I can’t quite reconcile carcinoid or even small-cell Ca with the ILD and honeycombing.
Small-cell Ca can be associated with paraneoplastic dermatomyositis and that may explain a lot of her skin and systemic symptoms though I don’t remember carcinoid causing anything like that.
I am certainly not a pathologist, but there appear to be some loosely formed granulomas in this biopsy. At least, I think there are some multinucleated giant cells.
How did the "real" pathologist read the biopsy?
Clinically, and based on the HRCT, this is scleroderma with some fibrosis. Although there is GGO on the HRCT, the BAL differential doesn't suggest a good response to steroids.
The path is interesting--it's difficult to identify any distinct air-spaces, and none of it looks like interstitial disease. Not too familiar with the special stains, but if they are for neuroendocrine cells I agree with the thought of carcinoid. Seems like that would be an incidental finding, however. Can this be positive in bronchoalveolar cell or small cell?
I agree with Mike L---I need some help from a pathologist on this one.
Some of you are on the right track. Key is the Chromogranin stains.
Here's what the pathologist said (which still doesn't necessarily give it away):
The submucosa contains a nests of ovoid to spindled cells that re immunoreacive for chromagranin and synaptophysin. Also present are minute fragments of relatively unremarkable alveolar parenchyma.
Now, I will tell you that it is not carcinoid. Have you ever seen carcinoid present in a way seen on the HRCT? Is carcinoid associated with scleroderma or crest?
Ont he other hand, the CT lung findings and the symptoms desribed in the case all occurred at the same time so they are likely related.
If this is a neuroendocrine tumor they can be associated with dermatomyositis and polymyositis and even SLE. You didn't describe any Gottron's nodules or heliotrope rash but these may account for the skin and systemic manifestations. However, I am not sure how to connect the neuroendocrine cells and the HRCT findings.
This is diffuse pulmonary neuroendocrin cell (PNEC) hyperplasia. It has been referred to as primary or as idiopathic.
There is hyperplasia and dysplasia of the lung's neuroendocrine cells - perhaps secondary to a preexisiting and non-related lung injury (Virchows Arch 1954 325:723). The result is numerous neuroepithelial bodies or "tumorlets" seen on biopsy, with those bodies staining positive for Chromogranin stains.
It is suggested presence of PNEC hyperplasia represents an adaptive or regenerative response to injury . Others have reported this condition developing without underlying lung disease (See Am J Surg Path 19:963 1995).
Epidemiologic studies have failed to show an association between PNEC and carcinoid tumors.
There is nothing in the literature about systemic scleroderma being associated with this condition, but I am assuming that is what this patient has. She will therefore be treated for her scleroderma and followed.
Interestingly, *cutaneous* scleroderma has been associated with carcinoid *syndrome*.....
I forgot to add that the H&E stains show the tumorlets nicely, in the submucosa. The other stains are merely confirming their neuroendocrine origin.
So, outside of the obviously "clear" association with Scleroderma, what is the significance of this pathology? Is this pathology of any significance? Does this require treatment, per se, or is it simply reflective of the underlying cause of injury which is, in this case, presumably the scleroderma?
There isn't enough in the literature to definitively nswer your question. The data that is available indicates that it does not progress, and that it does not become a carcinoid or small cell. Beyond that, I think the patient will be treted for the scleroderma and watched closely for any lung worsening (symptoms, PFT;s or radiographic progression).
Post a Commenttest post a comment